Intestinal Segments and Urinary Diversion
Jump to navigation
Jump to search
Surgical Anatomy[edit | edit source]
Stomach[edit | edit source]
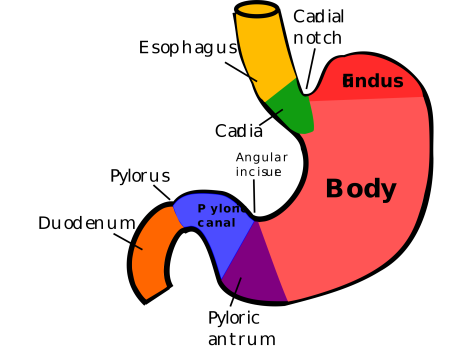
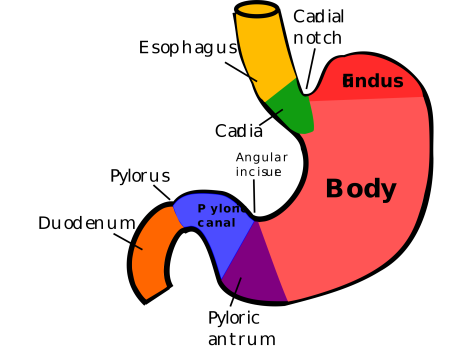
Regions of stomach. Source: Wikipedia
- Vascular organ
- Arterial blood supply
- Primarily from 3 branches of the celiac trunk
- Left gastric artery
- Supplies the lesser curvature
- Hepatic artery
- Gives off the right gastric artery, which also supplies the lesser curve of the stomach, and the gastroduodenal artery, which supplies the antrum and duodenum before giving off the right gastroepiploic artery.
- The splenic artery
- Gives off the vasa brevia (short gastrics), which supply the fundus and cardia, and the left gastroepiploic artery.
- Left gastric artery
- Primarily from 3 branches of the celiac trunk
- When a wedge of fundus is used, it should not include a significant portion of the antrum and should never extend to the pylorus or all the way to the lesser curve of the stomach.
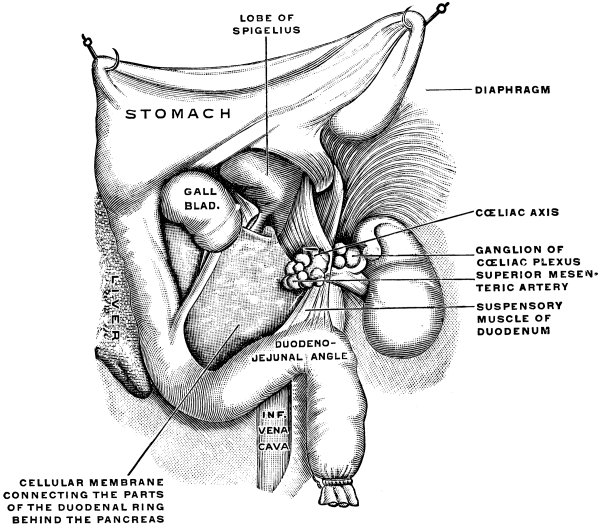
 Blood supply of stomach. Source: Wikipedia
Blood supply of stomach. Source: Wikipedia - The right gastroepiploic artery meets with the left gastroepiploic artery; both supply collateral flow to the greater curve of the stomach. By use of the gastroepiploic vessels, a pedicle of stomach may be mobilized as far as the pelvis
Small bowel[edit | edit source]
- ≈22 feet in length; however, may vary from 15-30 feet in length
- Differences between ileum and jejunum (5):
- Ileum
- More distal
- Small diameter
- Multiple arterial arcades
- Smaller arcade vessels
- Thicker mesentery
- Jejunum
- More proximal
- Larger diameter
- Single arterial arcades
- Larger arcade vessels
- Thinner mesentery
- Ileum
- The arcades receive their blood from the superior mesenteric artery
- Experimentally, up to 15 cm of small bowel can survive laterally to a straight vessel. In general, however, it should be assumed > 8 cm of small bowel will not survive away from a straight vessel
- In a post pelvic radiation patient, avoid use of 2 segments of the small bowel that may have been exposed to irradiation
- Last 2 inches of the terminal ileum
- 5 feet of small bowel beginning ≈6 feet from the ligament of Treitz (also known as the suspensory ligament of the duodenum), a thin muscle connecting the junction between the duodenum, jejunum, and duodenojejunal flexure to connective tissue surrounding the superior mesenteric artery and celiac artery
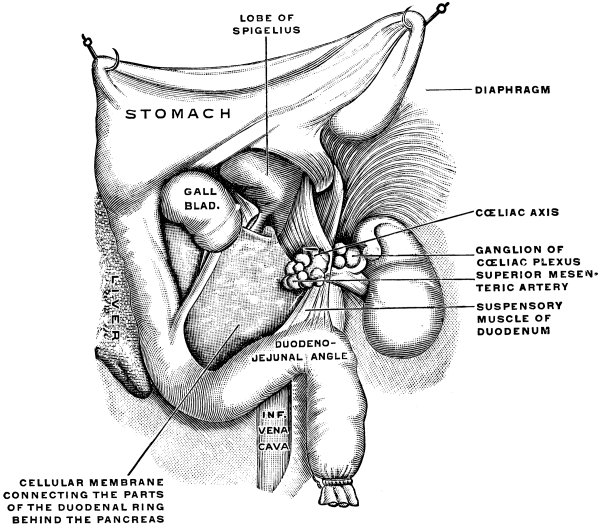
Ligament of Treitz. Source: Wikipedia
Colon[edit | edit source]
- The large bowel is divided into the:
- Cecum
- Ascending colon
- Transverse colon
- Descending colon
- Sigmoid colon
- Rectum
- The ascending colon is fixed to the right posterior abdominal wall to the level of the hepatic flexure, at which point the hepatocolic ligament secures this portion of the colon to the liver.
- The transverse colon lies free within the abdominal cavity and is fixed in the left upper quadrant at the splenic flexure by the phrenocolic ligament. The transverse colon is attached to the stomach by the gastrocolic omentum.
- Omentum flap should be based off of blood supply from the right gastroepiploic artery
- The right and left gastroepiploic arteries supply the greater curvature and the omentum.
- The pedicle can be based on either the right or left gastroepiploic artery; however, the caliber of the right gastroepiploic artery is usually larger, thus favoring its use.
- Omentum flap should be based off of blood supply from the right gastroepiploic artery
- The descending colon is fixed to the left lateral abdominal wall
- The sigmoid colon may or may not lie free within the abdominal cavity
- Arterial blood supply
- The colon receives its blood supply from the superior mesenteric artery, inferior mesenteric artery, and internal iliac arteries. The major arteries supplying the colon and rectum include the ileocolic, right colic, middle colic, left colic, sigmoid, superior hemorrhoidal, middle hemorrhoidal, and inferior hemorrhoidal arteries.
- INSERT FIGURE
- Weak points involving the vascular supply to the colon (3):
- Between the junction of the sigmoid and superior hemorrhoidal (Sudeck critical point) arteries
- Midpoints between the middle colic and right colic arteries
- Midpoint between the middle colic and left colic arteries (not shown in above diagram, but left colic artery is first branch of IMA (also not shown) and supplies the marginal artery§)
- Although anastomoses in these areas usually heal well, provided the principles of proper technique are followed, it is recommended to select an area for the anastomosis to one side of these points
- Venous drainage
- The inferior mesenteric vein drains into splenic vein.
- The superior mesenteric vien combines with the splenic vein to form the hepatic portal vein
- INSERT FIGURE
Bowel Preparation[edit | edit source]
Normal bowel bacterial flora[edit | edit source]
- Consists of:
- Aerobic organisms
- Most common: Escherichia coli and Enterococcus faecalis
- Anaerobic organisms
- Most common: Bacteroides and Clostridium
- Aerobic organisms
- Bacterial concentration ranges from
- 10-10e5 organisms per gram of fecal content in the jejunum
- 10e5-10e7 in the distal ileum
- 10e6-10e8 in the ascending colon
- 10e10-10e12 in the descending colon
Rationale for Bowel Preparation[edit | edit source]
- Solid feces may place strain on the anastomosis in the early phase of healing and result in ischemia with subsequent perforation
- In experimental animals, an anastomosis with vascular compromise at the anastomotic line, which would normally result in perforation, heals if the bowel has been properly prepared with antibiotics
- Infectious complications after radical cystectomy that are a direct result of fecal contamination include
- Peritonitis
- Intra-abdominal abscesses
- Wound dehiscence
- Anastomotic dehiscence
- Systemic sepsis
Classification (2)[edit | edit source]
- Mechanical vs. antibiotic
Mechanical (whole-gut irrigation)[edit | edit source]
- Reduces the amount of feces/total number of bacteria but not their concentration
- Can be done with polyethylene glycol (PEG)–electrolyte solution
Efficacy[edit | edit source]
- 2011 Cochrane review: Mechanical bowel preparation for elective colorectal surgery
- 18 trials with 5,805 participants were analyzed
- No difference in anastomotic leakage or wound infection rates; important to note that many of these studies involved peri-operative intravenous antibiotics and likely crucial in keeping the complication rate low
- Güenaga, Katia F., Delcio Matos, and Peer Wille‐Jørgensen."Mechanical bowel preparation for elective colorectal surgery." Cochrane Database of Systematic Reviews 9 (2011)
- No studies have adequately assessed the safety of omitting mechanical bowel preparation in urologic reconstructive surgery
Contraindications (5):[edit | edit source]
- Obstructed bowel
- Unstable cardiovascular system
- Congestive heart failure
- Cirrhosis
- Severe CKD
Adverse Events[edit | edit source]
- Hypokalemia
- Vigorous bowel cleansing, even with Go-Lytely or other electrolyte solutions, will often result in low potassium.
- Characteristic signs include muscular weakness with poor respiratory effort causing decreased ventilation in the presence of a normal chest x-ray.
- Vigorous bowel cleansing, even with Go-Lytely or other electrolyte solutions, will often result in low potassium.
- Diarrhea
Antibiotic[edit | edit source]
- Reduces the bacterial concentration
- PERIoperative IV antibiotics appear to be the most important means of preventing infectious complications of intestinal surgery.
- Systemic antibiotics must be given before the operative event if they are to be effective.
- A randomized trial in elective colorectal surgery found that PREoperative antibiotics did not reduce the risk of clinical infections§
- If perioperative antibiotics are given, they should be effective against anaerobes because it is complications from these organisms against which perioperative antibiotics appear to be particularly effective.
- Systemic antibiotics must be given before the operative event if they are to be effective.
Adverse Events[edit | edit source]
- Diarrhea
- Pseudomembranous enterocolitis
- Treatment involves the administration of vancomycin or metronidazole and discontinuance of other antibiotics that the patient is receiving
Indications for Urinary Diversion after Cystectomy[edit | edit source]
- Diseased bladder
- Dysfunctional bladders that result in persistent bleeding
- Obstructed ureters
- Poor compliance with upper tract deterioration
- Inadequate storage with total urinary incontinence
- Before transplantation in a patient who has a bladder that cannot adequately receive the transplant ureter
Selecting the segment of intestine[edit | edit source]
- Intestinal segments used most often for urinary tract reconstruction (2):
- Ileum
- Colon
- Jejunum is usually not used for reconstruction of the urinary system because it may result in severe electrolyte imbalance
- Although the same electrolyte abnormalities are possible with either ileum or colon, nutritional problems (Vitamin B12 deficiency and bile acid salt absorption) are less with colon when compared to ileum as long as the ileocecal valve is left intact
- Jejunum is usually not used for reconstruction of the urinary system because it may result in severe electrolyte imbalance
Ileal Conduit[edit | edit source]
- Simplest type of conduit diversion to perform; fewest intraoperative and immediate postoperative complications
Contraindications (3):[edit | edit source]
- Short bowel syndrome
- Inflammatory small bowel disease
- History of extensive pelvic irradiation where the ileum may have been affected
Summary of steps[edit | edit source]
- A segment 10-15 cm in length is selected 10-15 cm from the ileocecal valve. The cecum and ileal appendage (i.e., that portion of the distal ileum fixed to the retroperitoneum) are mobilized. The ileal mesentery is transilluminated, and a major arcade to the segment selected identified. With a mosquito clamp, the mesentery immediately beneath the bowel is penetrated, and the bowel is encircled with a vessel loop. An area at the base of the mesentery that is to one side of the feeding vessel is selected, and a second vessel loop is placed through the mesentery. At this juncture, the peritoneum overlying both sides of the mesentery is incised from bowel vessel loop to the base of mesentery vessel loop. With mosquito clamps, the tissue is clamped, severed, and tied with 4-0 silk. A portion of mesentery 2 cm in length is cleaned away from the bowel beneath the mesenteric incision. This procedure is repeated at the other end of the selected segment. The base of the mesentery should be as wide as possible and the mesenteric windows not excessive (in general about 5 cm in length) to prevent ischemia of the segment. Allen clamps are placed across the bowel in an angled fashion such that the antimesenteric portion is shorter than the mesenteric portion. (Some prefer to transect the bowel with an anastomotic stapler.) Thus a triangular piece of bowel is removed and discarded.
- The isolated ileal segment is placed caudad, and an ileoileostomy is performed as described earlier. The mesenteric window of the ileoileostomy is closed with interrupted 3-0 silk sutures. The isolated segment is then flushed with copious amounts of saline until the irrigant is clear, at which point the ureters are brought out the retroperitoneum in the right lower quadrant. To accomplish this, the left ureter must be brought over the great vessels and posterior to the sigmoid mesentery to the rent in the posterior peritoneum. This may be done by mobilizing the cecum cephalad to identify the right ureter. The left ureter may be identified by incising the line of Toldt of the left descending colon (Fig. 97-35). This dissection allows anastomosis of the ileal segment as proximally as needed to the ureter. Indeed, the ileum may be anastomosed directly to the renal pelvis on both sides if necessary (see Fig. 97-35C). After a cystectomy, the ureters are identified caudad to the iliac vessels and may be conveniently traced cephalad similar to the previous description. The ureteroileal anastomoses are performed as described previously. These anastomoses are stented
- The base of the conduit is fixed to the retroperitoneum in the right lower quadrant by suturing the posterior peritoneum to the conduit, thus effectively retroperitonealizing the ureterointestinal anastomosis.
Colon Conduit[edit | edit source]
- Commonly used colon conduits: transverse, sigmoid, and ileocecal
Transverse colon[edit | edit source]
- Used in patients with prior extensive pelvic irradiation or when an intestinal pyelostomy needs to be performed.
Sigmoid conduit[edit | edit source]
- Good choice in patients undergoing a pelvic exenteration who will have a colostomy since no bowel anastomosis needs to be made.
- Contraindications:
- When the internal iliac artery has been ligated and the rectum has been left in situ
- Extensive pelvic irradiation
Ileocecal conduit[edit | edit source]
- Advantages:
- Provides a long segment of ileum when long segments of ureter need replacement
- Provides colon for the stoma
Contraindications (3):[edit | edit source]
- Presence of inflammatory large bowel disease
- Disease of segement being considered
- Severe chronic diarrhea
Jejunal Conduit[edit | edit source]
- Advantages
- Avoids irradiated bowel and ureter
- Disadvantage:
- May result in severe electrolyte imbalance
- Rarely used except when neither colon or ileum can be used
- May result in severe electrolyte imbalance
Stomach Conduit[edit | edit source]
- Rarely indicated; may be considered when the use of other intestinal segments in a patient with a decreased amount of intestine would result in serious nutritional problems
- Advantages (5):
- Electrolyte imbalances rarely occur in patients with normal renal function, although a hypochloremic, hypokalemic, metabolic alkalosis has been described
- Less permeable to urinary solutes
- Has a net excretion of chloride and hydrogen ions rather than a net absorption of them, effectively reversing the acidosis of renal insufficiency; may be preferred option in patients with pre-existing metabolic acidosis or renal dysfunction
- Not associated with malabsorption; may be preferred option in patients with short bowel syndrome
- Not usually in field of radiation, may be preferred option in patients with previous pelvic radiation
- Produces less mucus
- Acidic pH reduces bacterial colonization
- Electrolyte imbalances rarely occur in patients with normal renal function, although a hypochloremic, hypokalemic, metabolic alkalosis has been described
- Complications specific to stomach conduit
- Early:
- Gastric retention
- Caused by atony of the stomach or edema of the anastomosis
- Hemorrhage
- Most commonly originating from the anastomotic site
- Hiccups
- Secondary to gastric distention
- Pancreatitis
- As a consequence of intraoperative injury.
- Gastroduodenal and gastroureteral leaks
- Have been reported, occasionally resulting in a fatal outcome
- Gastric retention
- Late:
- Dumping syndrome
- Steatorrhea
- Small stomach syndrome
- Increased intestinal transit time
- Bilious vomiting
- Afferent loop syndrome
- Hypoproteinemia
- Hematuria-dysuria syndrome (from the excreted acid)
- Severe metabolic alkalosis associated with respiratory distress
- The syndrome of severe metabolic alkalosis in patients who have had a gastrocystoplasty is most likely to occur in patients who have elevated gastrin levels
- Megaloblastic or iron deficiency anemia
- Severe ulcerative complications
- Rare
- Long-term histamine (H2) or proton-pump inhibition should be considered for these patients.
- Early:
Ileal vesicostomy[edit | edit source]
- Uses spatulated ileum and a generous transverse cystotomy to decompress the bladder and to allow an appliance to be used on the abdomen.
- Particularly well suited to spinal cord injury patients or those with significant neurologic disease.
- Patients who are particularly good candidates are those with significant detrusor–external sphincter dyssynergia.
- Concept is that patients with a neurogenic bladder have an easier job of caring for themselves with an abdominal stoma.
Intestinal Anastomoses[edit | edit source]
- Principles of intestinal anastomoses (6):
- Adequate exposure
- Adequate blood supply
- Prevention of local spillage or enteric contents
- Serosal apposition (watertight, without tension)
- Don’t tie suture so tightly that the tissue is strangulated
- Realignment of the mesentery of the two segments of bowel to be joined
- Types of anastomoses
- Intestinal anastomoses may be performed with use of sutures or staples
- Stapled bowel anastomoses have been shown to be as efficacious as hand-sewn anastomoses because both have similar complication rates
- Leak and fistula rate of 2.8% for stapled and 3% for sutured anastomoses
- Theoretical benefits of a stapled anastomosis:
- Provides for a better blood supply to the healing margin
- Reduced tissue manipulation
- Minimal edema with uniformity of suture placement
- Wider lumen is constructed
- Greater ease and less time involved in performing the anastomosis, and the length of postoperative paralytic ileus is reduced.
- Stapled bowel anastomoses have been shown to be as efficacious as hand-sewn anastomoses because both have similar complication rates
- Sutured anastomoses [Further details in Campbell’s]
- Enteroenterostomy by a Two-Layer Suture Anastomosis
- Enteroenterostomy by a Single-Layer Suture Anastomosis
- End-to-Side Ileocolic Sutured Anastomosis
- Ileocolonic End-to-End Sutured Anastomosis with Discrepant Bowel Sizes
- Stapled anastamoses [Further details in Campbell’s]
- See video on YouTube (sign-in required to verify age)
- Staples should not be used in bowel segments exposed to urine due to the potential for stones to form; rather, absorbable suture should be used for this
- The TA (transverse anastomosis) stapled anastomosis everts the suture line. Because staples close in a B configuration and do not crush the tissue, theoretically they prevent ischemia at the suture line.
- The anastomotic stapler places two linear double rows of staggered staples. When the knife is advanced, the staple line is divided. The height of the staples is also chosen according to the tissue to be transected. Most intestinal anastomoses are performed with medium staples, which have a closed height of ≈1.5 mm (open height of 3.5 mm).
- Ileocolonic Anastomosis with the Circular Stapling Device
- Side-to-side Stapled Anastomosis
- End-to-End Stapled Anastomosis: Ileal-Ileal or Ileocolonic Anastomosis
- Summary of steps:
- The antimesenteric border of the two bowel segments to be joined is approximated with a 3-0 silk suture 5 to 6 cm from the cut ends of the bowel. A holding suture is placed through both segments of bowel at their cut ends at the midpoint of the antimesenteric borders. Stay sutures are placed at the mesenteric border of each bowel segment, and two other sutures midway between the mesenteric and antimesenteric border on the lateral aspects of the bowel are also placed. The anastomotic stapler is positioned in the lumens of both segments of bowel along the antimesenteric border. The antimesenteric holding suture is pulled up adjacent to the stapler. The anastomotic stapler is locked in place, the staples are fired, and the knife is advanced. The staple lines are inspected for bleeders, which if persistent should be suture ligated with an absorbable suture. It is important for several 3-0 silk sutures to be placed at the apex of the stapled and cut antimesenteric incision. At this point, slight tension on the anastomotic line can place undue stress on the staple margin and cause a leak. The holding sutures are held up, and a linear stapler is placed across the open end of bowel and fired. Care must be taken so that the staples include the serosa in its entire circumference. Excess bowel tissue is excised flush with the instrument before it is disengaged. The mesentery is then reapproximated.
- Summary of steps:
- Laparoscopic and Robotic Anastomoses
- Compression Anastomoses and the Biofragmentable Ring
- Complications
- The most common cause of mortality and morbidity within the immediate postoperative period in urologic procedures in which gut is used relates to complications involving the bowel
- Factors that significantly contribute to anastomotic breakdown include:
- Poor blood supply
- Local sepsis induced by fecal spillage
- Drains placed on an intra-abdominal anastomosis
- Anastomosis performed in irradiated bowel
- Prior radiation significantly increases the likelihood of serious complications after radical cystectomy
- Complications of bowel anastamosis:
- Leakage of fecal contents
- Sepsis
- Wound infections
- Abdominal abscesses
- Hemorrhage
- Anastomotic stenosis
- Bowel obstruction
- Postoperative bowel obstruction is most common when the ileum is used for diversion
- The most common cause of post-operative bowel obstruction is adhesions, followed by recurrent cancer
- Pseudo-obstruction of the colon (Ogilvie syndrome)
- Usually occurs within the first 3 days postoperatively in patients with multiple medical illnesses
- Cause is not understood
- Patient develops severe abdominal pain, and a radiograph of the abdomen reveals a dilated cecum.
- Fistulas
- Two typyes occur in the postoperative period, fecal and urinary. These generally occur within the first several weeks after the operative event.
- Wound dehiscence
- May complicate the immediate postoperative period.
- Complications of the isolated intestinal segment
- Strictures of intestinal segments
- Elongation of the segment, occasionally resulting in massive enlargement
- When this occurs in conduits or ureteral substitutes, there is usually a distal obstruction
- In continent diversions, it may signal failure to catheterize the pouch frequently enough.
- If allowed to persist, the increased pressure may result in deterioration of renal function.
- Enlargement and elongation of the intestine may also result in a volvulus of the segment
- Intestinal anastomoses may be performed with use of sutures or staples
Abdominal Stoma[edit | edit source]
- Two types of stomas may be made on the anterior abdominal wall: flush with the skin and those that protrude.
- The flush stoma is preferable for the continent type of diversion in which intermittent catheterization is carried out and over which a small dressing is placed.
- The stoma that protrudes is preferable when a collection device is worn. A properly protruding stoma worn with an appliance results in a lesser incidence of stomal stenosis and a better appliance fit with fewer peristomal skin problems.
- The site of the stoma should be selected preoperatively. This is done by marking the stomal site with the patient in the sitting position, as well as in the supine position
- All stomas should be placed through the belly of the rectus muscle
- If the stoma is placed lateral to the rectus sheath, a parastomal hernia is likely to occur.
- The stoma should be brought through a circular incision made at the predetermined site.
- Paraplegics, often with abdominal prolapse and wheel-chair existence pose a special problem for stomal site selection. A right lower quadrant site often results in a stoma that is difficult for the patient to see, with the stoma and appliance squeezed between the abdomen and thigh. For this reason, in the paraplegic patient, the stoma should always, if possible, be placed in the upper abdomen [SASP 2014]
- Nipple Stoma: “Rosebud”
- Summary of Steps:
- A Babcock clamp is placed through the opening, and the bowel is grasped and brought out for a distance of 5 to 6 cm to make a nipple of about 2 to 3 cm in length. Two 3-0 chromic sutures are placed through the seromuscular layer of the bowel and the peritoneum on the anterior abdominal wall. Alternatively, the serosa may be sutured to the fascia with two 2-0 chromic sutures. The mesentery is aligned in its normal anatomic direction before the serosa is sutured to the peritoneal wall. The ileum is usually curved in a concave manner toward the mesentery. If the curvature is severe, the mesentery may be partially incised 1 cm from the bowel wall. Thus a portion of mesentery is preserved along the entire length of the bowel. This should straighten the curve in the bowel significantly if not completely. Four 3-0 chromic sutures are placed in quadrants through the full thickness of the bowel edge and through the seromuscular layer of the bowel 3 to 4 cm from the cut edge and then through the subcuticular skin layer. Sutures should not traverse the full thickness of the skin but should be placed through the subcuticular and subdermal layers only.
- When the sutures are tied, the bowel is everted and forms a nipple. A more secure nipple may be made by performing multiple myotomies through the seromuscular layer of the bowel above the skin line before construction of the nipple. The myotomies adhere serosa to serosa and reduce the risk of stomal retraction. This is particularly appropriate for patients who are obese
- Summary of Steps:
- Flush Stoma [Further details in Campbell’s]
- Loop End Ileostomy [Further details in Campbell’s]
- Easier to perform than the ileal end stoma in the patient who is obese
- Complications of Intestinal Stomas
- Early complications of abdominal stomas include:
- Stomal stenosis (most common)
- Leaving a catheter through the superficial portion of stoma nightly may reduced the need for operative revision of stomal stenosis
- Most likely cause of elongated dilated conduit with hydronephrosis and hyperchloremic acidosis
- Stomal retraction
- Stomal prolapse
- Parastomal hernia
- More common with loop than end-on stomas
- Most effective management is relocation of the stomal site to the other side of the abdominal wall and by closure of the hernia.
- Bowel necrosis
- Bleeding
- Bleeding that is extremely difficult to manage may be a result of cirrhosis and varices. In this situation, life-threatening bleeding from the stoma or conduit may occur. To stop the bleeding, portal decompression may be required
- Dermatitis
- Obstruction
- Stomal stenosis (most common)
- Early complications of abdominal stomas include:
Ureterointestinal Anastomoses[edit | edit source]
- The ureter may be anastomosed to the small bowel or colon or in a refluxing or non-refluxing anastomosis. There is controversy as to whether there is a benefit for either approach
- Methods of ureterocolonic anastomoses
- Leadbetter-Clarke technique
- Strickler technique
- Pagano technique
- Transcolonic Technique of Goodwin
- Cordonnier and Nesbit Techniques
- Small bowel anastomoses
- Bricker Technique
- See Figure
- A refluxing end-to-side ureter–small bowel anastomosis
- Relatively simple to perform
- Low complication rate
- Stricture rate is ≈6%
- Leak rate is ≈3% in the absence of stents, negligible with stents
- Summary of Steps:
- Excise a small button of seromuscular tissue and mucosa, spatulate the ureter for 0.5 cm, and suture the full thickness of the ureter to the full thickness of the bowel (i.e., mucosa and seromuscular layer to ureteral wall) with either interrupted or running 5-0 PDS. The anastomosis is stented with a soft Silastic catheter.
- Wallace technique
- See Figure
- A refluxing end-to-end ureter-small bowel anastomosis
- Lowest complication rate of any of the ureterointestinal anastomotic techniques.
- Not recommended for patients who have extensive carcinoma in situ or who have a high likelihood of recurrent tumor in the ureter.
- A recurrence of tumor at the anastomotic line in one ureter would block both ureters, causing uremia from bilateral obstruction.
- Other techniques described in Campbell’s: Le Duc technique (non-refluxing, laid down on ileal track), tunneled Small Bowel Anastomosis, Split-Nipple technique, Hammock anastomosis, Ureteral dipping technique, Ureter–Small Bowel Anastomosis Using Serosal Compression of the Extramural Ureter as an Antireflux Mechanism
- Bricker Technique
- Intestinal Antireflux Valves
- The ureter is sutured by the technique of either Bricker or Wallace (as described earlier) to the end of the bowel, and the bowel is used to make a one-way valve.
- Three basic types of antireflux mechanisms commonly used with the bowel:
- Ileocecal intussusception
- Ileoileal intussusception
- Ileal nipple valve placed into colon.
- Complications of ureteroinstestinal anastamoses (5):
- Leakage (fistula)
- Typically occur within the first 7-10 days postoperatively
- May cause periureteral fibrosis and scarring with subsequent stricture formation.
- Incidence of 3-9%; can be reduced nearly to 0 if soft Silastic stents are used.
- Soft Silastic stents are effective in reducing the leak rate, subsequent stricture formation, and postoperative complications.
- Stricture
- One of the most difficult complications of ureterointestinal anastomoses
- In general, strictures are caused by ischemia, a urine leak, radiation, or infection. Anti-refluxing techniques have a higher incidence of stricture.
- Ureteral strictures can also occur away from the ureterointestinal anastomosis. This stricture is most common in the left ureter and is usually found as the ureter crosses over the aorta beneath the inferior mesenteric artery.
- This may occur because of overly aggressive stripping of adventitia and angulation of the ureter at the inferior mesenteric artery.
- Treatment options include endoscopic, interventional radiology, open surgery techniques
- See Management of Upper Urinary Tract Obstruction Chapter Notes
- The most successful technique is re-exploration, with removal of the stenotic segment and reanastomosis of the ureter to the bowel.
- Strictures with less favorable outcomes with endourologic methods:
- Occurring < 1 year from the original procedure
- Strictures ≥1.5 cm (Chapter 49 describes 1.0 and 2.0cm cut-offs)
- Left-sided strictures
- Renal function deterioration
- Usually a consequence of lack of ureteral motility, infection, or stones but can be caused by obstruction at the ureteral-intestinal anastomosis.
- Acute pyelonephritis
- Occurs both in the early postoperative period and during the long term
- Incidence 10-20% with ileal conduits and 9% with antirefluxing colon conduits
- Reflux in those anastomoses that were performed to prevent reflux
- Leakage (fistula)
Postoperative care[edit | edit source]
- The use of nasogastric or gastrostomy decompression during the postoperative period of ileus is somewhat controversial.
- The use of a nasogastric tube in the postoperative period reduces postoperative vomiting.
- The fluid lost via a nasogastric tube used to manage paralytic ileus is isotonic and alkaline. Therefore, this should be replaced with Lactated Ringer's§ that also provides replacement with approriate levels of potassium, chloride, and bicarbonate.
- Saline with KCl supplementation would be more appropriate for replacement of gastric secretions.
- Diet
- Clear liquids may be begun when the paralytic ileus resolves and bowel activity resumes. If clear liquids are tolerated, the diet may be advanced. This sequence of events generally takes 1-4 days.
- If the nutritional condition of the patient is impaired preoperatively, a postoperative complication delays oral feeding, or the paralytic ileus is still present on the 5th postoperative day, the patient should receive IV nutrition.
- It is preferable to begin the hyperalimentation the day after surgery if any of these complications are anticipated.
- If the nutritional condition of the patient is impaired preoperatively, a postoperative complication delays oral feeding, or the paralytic ileus is still present on the 5th postoperative day, the patient should receive IV nutrition.
- Clear liquids may be begun when the paralytic ileus resolves and bowel activity resumes. If clear liquids are tolerated, the diet may be advanced. This sequence of events generally takes 1-4 days.
- Enhanced recovery after surgery (ERAS) protocols aim to improve surgical outcomes by reducing variation in perioperative best practices.
- 2016 meta-analysis
- 13 studies
- Results
- ERAS was associated with reduced complication rates, time to return of bowel function, and shorter LOS.
- No difference in overall readmission rates, though slightly reduced readmissions at 30 days in the ERAS group.
- Tyson, Mark D., and Sam S. Chang. "Enhanced recovery pathways versus standard care after cystectomy: a meta-analysis of the effect on perioperative outcomes." European urology 70.6 (2016): 995-1003
- 2016 meta-analysis
Complications of urinary intestinal diversion[edit | edit source]
- See Video Review (Dr. John Phillips)
- 3 categories: metabolic, neuromechanical, and technical-surgical
- Metabolic complications result from altered solute reabsorption by the intestine of the urine that it contains
- Neuromechanical aspects involve the configuration of the gut, which affects storage volume and contraction of the intestine that may lead to difficulties in storage.
- Technical-surgical complications involve aspects of the procedure that result in surgical morbidity
Metabolic[edit | edit source]
- LSD ORGASMIC (9):
Lytes[edit | edit source]
- Factors that influence the amount of solute and type of absorption are:
- Segment of bowel used
- Surface area of the bowel
- Amount of time the urine is exposed to the bowel
- Concentration of solutes in the urine
- Renal function
- pH of the fluid
INSERT TABLE
- Stomach conduit
- Electrolyte imbalances rarely occur in patients with normal renal function. However, hypochloremic, hypokalemic metabolic alkalosis can occur in patients with concomitant renal failure.
- Symptoms of this include lethargy, respiratory insufficiency, seizures, and ventricular arrhythmias may occur.
- Patients are usually successfully treated with an H2 blocker to reduce proton secretion by the gastric segment and rehydration.
- Electrolyte imbalances rarely occur in patients with normal renal function. However, hypochloremic, hypokalemic metabolic alkalosis can occur in patients with concomitant renal failure.
- Jejunal conduit
- Hypochloremic, hyperkalemic, hyponatremic metabolic acidosis can occur.
- Symptoms of this include lethargy, nausea, vomiting, dehydration, muscle weakness, and elevated temperature.
- May be exacerbated by administration of hyperalimentation solutions.
- The severity of the syndrome depends on the location of the segment of jejunum that is used. The more proximal the segment, the more likely the syndrome is to develop.
- Treatment is rehydration with sodium chloride and correction of the acidosis with sodium bicarbonate.
- Provided that renal function is normal, the hyperkalemia is corrected by renal secretion.
- A thiazide diuretic may be helpful to correct the hyperkalemia (recall side effects of thiazides: 3 hypers and 3 hypos: hyperglycemia, hyperlipidemia, and hyperuricemia with hypokalemia, hypocitraturia, and hypomagnesuria with metabolic alkalosis).
- After restoration of normal electrolyte balance, long-term therapy involves oral supplements with sodium chloride and a thiazide diuretic, if needed.
- Hypochloremic, hyperkalemic, hyponatremic metabolic acidosis can occur.
- Ileum or colon conduit
- Hyperchloremic metabolic acidosis can occur.
- Symptoms of this include lethargy, easy fatigability, anorexia, weight loss, and polydipsia.
- The mechanism of hyperchloremic metabolic acidosis is a result of the ionized transport of ammonium
- Treatment involves alkalizing agents or blockers of chloride transport.
- ≈16% of patients with ileal conduits will develop metabolic acidosis requiring treatment.
- Alkalinization with oral sodium bicarbonate is effective in restoring normal acid-base balance.
- Potassium citrate, sodium citrate, and citric acid solution (Polycitra) may be used instead if excessive sodium administration is a problem because of cardiac or renal disease and if potassium supplementation is desirable or at least not harmful.
- Hyperchloremic metabolic acidosis can occur.
- Hypokalemia and total-body depletion of potassium may occur in patients with urinary intestinal diversion [though hyperkalemia with jejunal conduit].
- More common in patients with ureterosigmoidostomies
- In treating these patients, if the hypokalemia is associated with severe hyperchloremic metabolic acidosis, treatment must involve both replacement of potassium and correction of the acidosis with bicarbonate
Altered Sensorium[edit | edit source]
- May occur as a consequence of magnesium deficiency, drug intoxication, or abnormalities in ammonia metabolism
- Ammoniagenic coma in patients with urinary intestinal diversion is most commonly associated with decreased liver function.
- Ammonium excreted by the kidneys is reabsorbed by the intestinal segment, and then returned to the liver via the portal circulation. The liver metabolizes ammonium to urea via the ornithine cycle.
- The liver usually adapts to the excess ammonia and rapidly metabolizes it; hepatic dysfunctionmay therefore result in ammoniagenic coma.
- Ammoniagenic coma can occur in patients with normal hepatic function.
- Systemic bacteremia, with endotoxin production, inhibits hepatic function and may precipitate this clinical entity. Urinary tract infections with urea-splitting organisms may also overload the ability of the liver to clear the ammonia.
- If this syndrome occurs in a patient suspected of having near normal hepatic function, systemic bacteremia or urinary obstruction should be suspected.
- Ammoniagenic coma can occur in patients with normal hepatic function.
- Prompt urinary drainage with treatment of the offending urinary pathogens along with systemic antibiotics and the administration of oral neomycin or lactulose to reduce absorption of ammonia in the gastrointestinal tract are the key components to patient management.
Abnormal Drug metabolism[edit | edit source]
- Drug intoxication can occur in patients with urinary intestinal diversion. Drugs more likely to be problematic are those absorbed by the gastrointestinal tract and excreted unchanged by the kidney. Thus, the excreted drug is re-exposed to the intestinal segment, which then reabsorbs it, and toxic serum levels develop. This has been reported with phenytoin, methotrexate, lithium and theophylline.
- Patients receiving chemotherapy who have intestine interposed in the urinary tract have increased toxic effects of chemotherapeutic agents. Although chemotherapy is usually well tolerated by patients with conduits, toxicity has been documented in a patient with an ileal conduit.
- In patients with continent diversions who are receiving chemotherapy, consideration should be given to draining the pouch while the toxic drugs are being administered.
Osteomalacia[edit | edit source]
- Osteomalacia or renal rickets occurs when mineralized bone is reduced and the osteoid component becomes excessive.
- Osteomalacia in urinary intestinal diversion may be caused by:
- Persistent acidosis
- Vitamin D resistance
- Excessive calcium loss by the kidney
- Treatment involves correction of the acidosis and dietary supplementation of calcium
- Patients who develop osteomalacia report lethargy, joint pain, especially in the weight-bearing joints, and proximal myopathy
Renal function deterioration[edit | edit source]
- ≈20% of patients experience significant and progressive renal function deterioration independent of the type of urinary diversion
- Incidence for both sepsis and renal failure are greater in patients with ureterosigmoidostomy than in those with conduits
- Most common cause of death in patients with ureterosigmoidostomy for > 15 years is acquired renal disease
- Incidence for both sepsis and renal failure are greater in patients with ureterosigmoidostomy than in those with conduits
- Renal function necessary for urinary intestinal diversion
- The amount of renal function required to effectively blunt the reabsorption of urinary solutes by the intestinal segment and to prevent serious metabolic side effects depends on the type of urinary intestinal diversion constructed (i.e., the amount of bowel to be used and the length of time the urine is exposed to the intestinal mucosa).
- A greater degree of renal function is necessary for continent diversions than for short conduit diversions.
- eGFR cut-off for continent diversion varies by source:
- Chapter 97: > 40ml/min
- Chapter 99: >35 – 40 mL/min
- 2019 AUA MIBC Guidelines: > 45 mL/min
- A patient with serum creatinine > 2 mg/dL (177 µmol/L) may be considered for a continent diversion if:
- Able to achieve a urine ≤ pH of 5.8 after an ammonium chloride load
- Able to achieve urine osmolality ≥ 600 mOsm/kg in response to water deprivation
- GFR > 35 mL/min
- Minimal protein in the urine
- A patient with serum creatinine > 2 mg/dL (177 µmol/L) may be considered for a continent diversion if:
- The amount of renal function required to effectively blunt the reabsorption of urinary solutes by the intestinal segment and to prevent serious metabolic side effects depends on the type of urinary intestinal diversion constructed (i.e., the amount of bowel to be used and the length of time the urine is exposed to the intestinal mucosa).
- Because urea and creatinine are reabsorbed by both the ileum and the colon, serum concentrations of urea and creatinine do not necessarily accurately reflect renal function
- Fractional excretion of sodium most accurately measures renal function in a patient with a urinary diversion.
Growth retardation[edit | edit source]
- Conduits have detrimental effect on linear growth and development. Patients are more susceptible to fractures and to complications after orthopedic procedures.
Acidosis/Alkalosis[edit | edit source]
- The ability to establish a hyperchloremic metabolic acidosis appears to be retained by most segments of ileum and colon over time.
Stones[edit | edit source]
- Risk factors for stone formation with urinary diversion
- Persistent infection, associated with the development of magnesium ammonium phosphate stones.
- Foreign body such as a staple or nonabsorbable suture, on which concretions form
- Alterations in bowel mucosa may also serve as a nidus for stone formation
- Alterations in intestinal mucus, particularly in the presence of infection or obstruction, may serve as a nidus or, more important, may interfere with emptying and thereby exacerbate infection and stone formation
Malabsorption[edit | edit source]
- In patients with a significant loss of ileum, there can be malabsorption of
- Vitamin B12 resulting in anemia and neurologic abnormalities
- Since the liver stores enough vitamin B12 to supply the body’s requirement for 3-5 years without oral intake, pathologic problems would not be expected to manifest themselves for many years
- Bile salts resulting in mucosal irritation and diarrhea because the ileum is the major site of bile salt reabsorption.
- There are 3 mechanisms of diarrhea in a patient with ileal conduit:
- Malabsorption of bile salts since the ileum is the major site of bile salt reabsorption
- Malabsorption of fat from loss of “ileal break" and small intestinal bacterial overgrowth from loss of ileocecal valve
- The ileal break is a mechanism whereby gut motility is reduced when lipids come in contact with the ileal mucosa so that increased absorption can occur. With the loss of ileum, the lipid does not result in decreased motility and is presented unmetabolized to the colon, which may cause fatty diarrhea.
- Loss of ileocecal valve
- May result in reflux of large concentrations of bacteria into the ileum, resulting in small intestinal bacterial overgrowth which may cause nutritional abnormalities that involve interference with fatty acid reabsorption and bile salt interaction.
- With the lack of absorption of fats and bile salts, these are presented to the colon and result in diarrhea.
- There are 3 mechanisms of diarrhea in a patient with ileal conduit:
- Vitamin B12 resulting in anemia and neurologic abnormalities
- Loss of a significant portion of jejunum may result in malabsorption of fat, calcium, and folic acid
- Loss of the colon may result in diarrhea because of lack of fluid and electrolyte absorption, loss of bicarbonate
Infections[edit | edit source]
- An increased incidence of bacteriuria, bacteremia, and septic episodes occurs in patients with bowel interposition.
- ≈75% of ileal conduit urine specimens are infected. Many of these patients, however, show no untoward effects and seem to do well with chronic bacteriuria.
- Deterioration of the upper tracts is more likely when the culture becomes dominant for Proteus or Pseudomonas. Thus patients with relatively pure cultures of Proteus or Pseudomonas should be treated, whereas those with mixed cultures may, in general, be observed, provided they are not symptomatic.
- Pouchitis
- Not uncommon, especially in the early postoperative period when mucous accumulation can be high.
- A simple program of mechanical irrigation can decrease the incidence of infections, though asymptomatic colonization may not decrease
- Pyocystis
- Ooccurs in ≈20% of patients who undergo supravesical diversion.
- Patients typically have a malodorous discharge and may develop sepsis.
- If conservative measures, such as routine bladder irrigations fail, vaginal vesicostomy (creation of a large vesico-vaginal fistula), is an effective method of preventing pyocystis in women. This is an especially good alternative for an elderly or high risk patient. Cystectomy is an effective treatment for pyocystis and would likely be required if the patient was a male
Cancer[edit | edit source]
- Bladder cancer after augmentation presents:
- At a younger age than is typical for bladder malignancies
- With atypical symptoms such as vague abdominal pain, urosepsis or increased frequency of urinary tract infection (UTI), difficult catheterization, and renal failure.
- With atypical signs such as new hydronephrosis and bladder wall thickening.
- Advanced disease
- Usually with a minimum 10-year lag time between augmentation and presentation of bladder malignancy.
- Most of the tumors are adenocarcinomas, but can also be adenomatous polyps, sarcomas, and urothelial carcinoma
- The incidence of cancer development in patients with ureterosigmoidostomy varies between 6-29%, mean 11%. Because its incidence is significant in patients with ureterosigmoidostomies, they should have routine colonoscopies on a scheduled periodic basis. Case reports of tumors developing in patients with ileal conduits, colon conduits, bladder augmentations, rectal bladder, neobladders, and ileal ureters have been described. When ureterointestinal anastomoses are defunctionalized, there remains a risk of adenocarcinoma in the defunctionalized diversion. Therefore, they should be excised rather than merely ligated and left in situ
False-positive pregnancy test[edit | edit source]
- Male and female patients with urinary diverison can have false positive urinary pregnancy tests, possibly due to the mucous produced§
Ruptured augmented bladder[edit | edit source]
- Up to 50% of cystogram studies in cases of a ruptured augmented bladder may be negative for the injury; therefore, a negative cystogram does not rule out a bladder rupture.
- Confirmation of suspected perforation of an augmented bladder is best achieved by performing a CT cystogram with a minimum of 300 ml of contrast placed in the bladder with a CT phase taken with the bladder distended and emptied.
Neuromechanical Aspects of Intestinal Segments[edit | edit source]
- 2 aspects of neuromechanical properties are important to urinary intestinal diversion: volume-pressure relationships and motor activity:
Volume-pressure considerations[edit | edit source]
- By splitting most segments, the volume increases by ≈50%. The goal in reconfiguring the bowel is to achieve a spheric storage vessel. This configuration has the most volume for the least surface area.
- Over time, the volume capacity of segments increases. This occurs only if they are frequently filled. Their volume decreases with time if they are nonfunctional
Motor activity[edit | edit source]
- It has been suggested that splitting the bowel on its antimesenteric border discoordinates motor activity and thereby causes a lesser intraluminal pressure. However, the literature is contradictory with respect to the effect of detubularization on segments of ileum and colon used to construct storage vessels for continent diversions.
- Thus, reconfiguring bowel usually increases the volume, but its long-term effect on motor activity and wall tension is unclear at this time. Some patients with orthotopic bladders after a number of years of spontaneous voiding require intermittent catheterization. In these patients the bowel segment has become flaccid, and the ability of the patient to generate intraluminal pressure by a Valsalva maneuver is limited.
Questions[edit | edit source]
- List 5 differences between the ileum and jejunum
- What is the safe maximum distance of bowel that will survive away from a straight vessel?
- What segments of bowel should be avoided in a patient with prior pelvic radiation?
- What are potential weak points in blood supply to the colon?
- What are potential advantages of a stomach conduit?
- Which bacterial flora are found in the bowel?
- What is the bacterial concentration in the jejunum? Distal ileum? Ascending colon? Descending colon?.
- What is the goal of mechanical vs. antibiotic bowel regimen?
- What are contraindications to whole-gut irrigation?
- What are the principles of intestinal anastomoses
- List contraindications to use of ileum for conduit.
- List contraindications to use of transverse, sigmoid, and ileocecal conduits.
- Which segment of bowel is associated with the highest rates of post-operative bowel obstruction?
- What are risk factors for bowel anastamosis breakdown?
- List 3 different techniques of anastomosing the ureter to the small bowel
- Which technique of anastomosing the ureter to the small bowel has the lowest complication rates?
- List complications associated with ureteroenteric anasmoses.
- List the metabolic complications of urinary intestinal diversion
- Which bowel segment used in urinary diversion is associated with elevated aldosterone? Elevated renin?
- What is the treatment of hypochloremic metabolic acidosis in a patient with an ileal conduit?
- What renal function parameters are recommended for patients undergoing continent diversion?
- List 3 mechanisms of diarrhea associated with ileal conduit
- What may deficiency may result from malabsorption when using jejunum for urinary diversion?
- What are the electrolyte derangements associated with:
- When should treatment of asymptomatic bacteruria in a urinary diversion be considered?
- What is the expected histology of a bladder cancer associated with urinary diversion?
Answers[edit | edit source]
- List 5 differences between the ileum and jejunum
- Ileum: more distal, smaller lumen, multiple arterial arcades, smaller arcade vessels, thicker mesentery
- Jejunum: more proximal, larger lumen, single arterial arcades, larger arcade vessels, thinner mesentery
- What is the safe maximum distance of bowel that will survive away from a straight vessel?
- 8cm
- What segments of bowel should be avoided in a patient with prior pelvic radiation?
- Last 2 inches of ileum
- 5 feet of small bowel beginning 6 feet from ligament of Treitz
- What are potential weak points in blood supply to the colon?
- Between middle colic and left colic
- Between middle colic and right colic
- Between sigmoidal and superior rectal (Sudeck point)
- What are potential advantages of a stomach conduit?
- Electrolyte imbalances rarely occur
- Not associated with malabsorption; may be preferred option in patients with short bowel syndrome
- Not usually in field of radiation, may be preferred option in patients with previous pelvic radiation
- Produces less mucus
- Acidic pH reduces bacterial colonization
- Which bacterial flora are found in the bowel?
- Aerobic: E. coli and enterococcus
- Anaerobic: bacteroides and clostridium
- What is the bacterial concentration in the jejunum? Distal ileum? Ascending colon? Descending colon?
- The bacterial concentration ranges from 10-105 organisms per gram of fecal content in the jejunum, 105-107 in the distal ileum, 106 -108 in the ascending colon, and 1010-1012 in the descending colon.
- What is the goal of mechanical vs. antibiotic bowel regimen?
- Mechanical: reduce bacterial load
- Antibiotic: reduce bacterial concentration
- What are contraindications to whole-gut irrigation?
- Obstructed bowel
- CHF
- Unstable cardiovascular system
- Cirrhosis
- Severe renal disease
- What are the principles of intestinal anastomoses
- Adequate exposure
- Adequate blood supply
- Prevention of local spillage or enteric contents
- Serosal apposition (watertight, without tension)
- Don’t tie suture so tightly that the tissue is strangulated
- Realignment of the mesentery of the two segments of bowel to be joined
- List contraindications to use of ileum for conduit.
- Short bowel syndrome
- Inflammatory bowel disease
- History of extensive pelvic radiation
- List contraindications to use of transverse, sigmoid, and ileocecal conduits.
- Presence of inflammatory large bowel disease
- Severe chronic diarrhea
- Which segment of bowel is associated with the highest rates of post-operative bowel obstruction?
- Ileum
- What are risk factors for bowel anastamosis breakdown?
- Poor blood supply
- Local fecal spillage
- Drain placed near anastamosis
- Radiation
- List 3 different techniques of anastomosing the ureter to the small bowel
- Bricker – end to side
- Wallace – end to end
- LeDuc – laid down on ileal track
- Which technique of anastomosing the ureter to the small bowel has the lowest complication rates?
- Wallace
- List complications associated with ureteroenteric anasmoses.
- Leakage
- Stenosis
- Renal insufficiency
- Reflux in those that were constructed with anti-reflux method
- Acute pyelonephritis
- List the metabolic complications of urinary intestinal diversion
- LSD ORGASMIC
- Lytes, Sensorium altered, Drug metabolism alterted, Osteomalacia, Renal function deterioration, growth suppression, acidosis/alkalosis, stones, malabsorption, infection, cancer
- Which bowel segment used in urinary diversion is associated with elevated aldosterone? Elevated renin?
- Elevated aldosterone: stomach
- Elevated renin: jejunum
- What is the treatment of hypochloremic metabolic acidosis in a patient with an ileal conduit?
- Sodium bicarb; can be substituted for potassium citrate if cardiac or renal disease preclude sodium or potassium substitution beneficial
- What renal function parameters are recommended for patients undergoing continent diversion?
- eGFR > 45 (AUA MIBC Guidelines)
- Minimal protein uria
- Urine pH ≤ pH of 5.8 after an ammonium chloride load
- Can achieve urine osmolality ≥ 600 mOsm/kg in response to water deprivation
- List 3 mechanisms of diarrhea associated with ileal conduit
- Bile salt malabsorption
- Fat malabsorption
- Loss of ileocecal valve
- What may deficiency may result from malabsorption when using jejunum for urinary diversion?
- Fat, calcium, folic acid
- What are the electrolyte derangements associated with:
- Ileal conduit: hyperchloremic, hypokalemic metabolic acidosis
- Jejunal conduit: hypochloremic, hyperkalemic metabolic acidosis
- Stomach conduit: hypochloremic, hypokalemic metabolic alkalosis
- When should treatment of asymptomatic bacteruria in a urinary diversion be considered?
- Pure proteus or pseudomonas in culture
- What is the expected histology of a bladder cancer associated with urinary diversion?
- Adenocarcinoma
References[edit | edit source]
- Wein AJ, Kavoussi LR, Partin AW, Peters CA (eds): CAMPBELL-WALSH UROLOGY, ed 11. Philadelphia, Elsevier, 2015, chap 97