Inguinal Node Dissection
Jump to navigation
Jump to search
See Contemporary management of patients with penile cancer and lymph node metastasis (Nat Rev Urol 2007)
Anatomic Considerations[edit | edit source]
Femoral Triangle[edit | edit source]
Borders[edit | edit source]
- Roof: fascia lata (covers femoral sheath)
- Fascia lata is continuous with external oblique aponeurosis superiorly[1]
- Floor: pectineus, iliopsoas, adductor longus muscles
- Superior: inguinal ligament (runs from anterior superior iliac spine to pubic tubercle)
- Inguinal ligament is the portion of the external oblique aponeurosis which extends between the anterior superior iliac spine and the pubic tubercle as a thick band, folded inward[2]
- Lateral: medial border of sartorius muscle
- Medial: medial border of adductor longus muscle
Contents[edit | edit source]
Lateral to medial: NAVEL
- Nerve
- Artery
- Vein
- Empty space
- Allows the veins and lymph vessels to distend to accommodate different levels of flow
- Lymph nodes
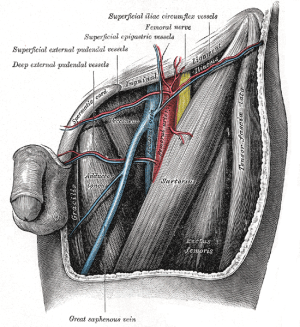
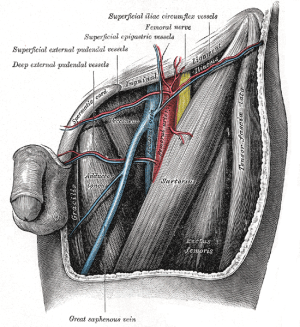
Left femoral triangle; source: Wikipedia
Nerves[edit | edit source]
- Femoral nerve
- Lies deep to the iliacus fascia
- Lateral to common femoral artery
- Functions
- Motor: innervates the pectineus, quadriceps femoris, and sartorius muscles
- Sensory: anterior thigh
- Should be preserved during inguinal dissection.
- Some of the sensory branches, however, are commonly sacrificed in the regional node dissection.
Vasculature[edit | edit source]
- Posterior to fascia lata
- Common femoral artery
- Continuation of external iliac artery
- External iliac artery above inguinal ligament, common femoral artery below inguinal ligament
- Gives off a branch called deep (profunda) femoral artery and continues as superficial femoral artery[3]
- Blood supply to the skin of the inguinal region is from branches of the common femoral artery.
- Complete inguinal dissection necessitates ligation of these branches.
- Viability of the skin flaps raised during the dissection depends on anastomotic vessels in the superficial fatty layer of the Camper fascia
- A transverse skin incision least compromises blood supply to the skin.
- Complete inguinal dissection necessitates ligation of these branches.
- Medial to femoral nerve
- Just medial to the midpoint of the inguinal ligament in the inguinal crease region[4]
- Continuation of external iliac artery
- Common femoral vein
- Deep femoral vein and Great saphenous vein (also known as long saphenous vein) empty into the common femoral vein
- Great saphenous vein approaches common femoral vein medially
- Deep femoral vein approaches common femoral vein laterally
- Medial to common femoral artery
- Deep femoral vein and Great saphenous vein (also known as long saphenous vein) empty into the common femoral vein
- Common femoral artery and common femoral vein are enclosed in femoral sheath[5]
Inguinal Lymph Nodes[edit | edit source]
- Classified as superficial vs. deep inguinal nodes
- Fascia lata of the thigh separates the superficial and deep inguinal nodes
- Superficial inguinal nodes
- Anatomic groups (5):
- Central nodes around the saphenofemoral junction
- Superolateral nodes around the superficial circumflex vein
- Inferolateral nodes around the lateral femoral cutaneous and superficial circumflex veins
- Superomedial nodes around the superficial external pudendal and superficial epigastric veins
- Inferomedial nodes around the greater saphenous vein
- Anatomic groups (5):
- Deep inguinal nodes
- Fewer in number, compared to superficial inguinal nodes
- Lie primarily medial to the femoral vein in the femoral canal
- Most cephalad of the deep inguinal nodes is the Node of Cloquet
- Node of Cloquet is located between the femoral vein and the lacunar ligament
- Lacunar ligament connects the inguinal ligament to the pectineal ligament
- Node of Cloquet is located between the femoral vein and the lacunar ligament
Penile Lymphatics[edit | edit source]
- Superficial lymphatic system
- Drains the prepuce and skin of the penile shaft
- Empties into the right and left superficial inguinal nodes
- Deep lymphatic system
- Drains the glans penis
- Empties into the superficial inguinal nodes and the deep inguinal nodes
- Primary site of metastatic spread of penile carcinoma occurs via the regional lymphatic system, first to the inguinal lymph node chain and then to the iliac and pelvic lymph nodes.
- Presence and extent of regional LN metastases is the single most important prognostic factor in determining the long-term survival of patients with penile cancer
- If cancer has spread to the pelvic nodes, long-term survival is < 10%
- Presence and extent of regional LN metastases is the single most important prognostic factor in determining the long-term survival of patients with penile cancer
- Inguinal metastatic spread can be unilateral or bilateral, and crossover drainage from the right to left groin or vice versa can also occur.
- Metastatic spread from the inguinal lymph nodes to the contralateral pelvis or from the right to left pelvis has never been reported.
- Skip lesions with direct lymphatic drainage from penile tumors to the pelvic lymph nodes has never been reported. .
- Further spread from the true pelvis to the retroperitoneal lymph nodes is beyond the regional drainage system of the penis and represents systemic metastatic disease
Inguinal Lymphadenectomy[edit | edit source]
Standard radical inguinal lymphadenectomy[edit | edit source]
- In the standard radical inguinal lymphadenectomy, both the superficial and deep inguinal lymph nodes are removed
- Superficial dissection removes nodes superficial to the fascia lata
Indications[edit | edit source]
- Clinically node-positive disease (palpable on physical exam)
- Clinically node-negative disease (not palpable on physical exam) but increased risk for inguinal metastasis based on primary tumor characteristics (pT ≥2, presence of vascular or lymphatic invasion, or grade ≥3).
- cN3 (fixed nodal mass) is managed initially with neoadjuvant chemotherapy followed by radical inguinal lymphadenectomy in responders
- May be curative when the disease is limited to the inguinal nodes.
Technique[edit | edit source]
- See BJUI Surgical atlas. Surgical management of penile carcinoma: the inguinal nodes
- Have available
- LigaSure™ Maryland jaw, 23cm length
- 2-0 silk ties for lymphatics
- 4-0 prolene on RB1 in case of vasculature injury
- Radical inguinal lymphadenectomy
- Boundaries of dissection:§
- Superior: inguinal ligament
- Medial: adductor longus muscle
- Lateral: sartorious muscle (saphenous vein and femoral vein in modified template)
- Inferior: apex of the femoral triangle/fossa ovalis (where the saphenous penetrates the fascia lata)
- Floor: pectineus muscle for deep dissection (fascia lata for superficial)
- Note that adductor longus and sartorious are posterior to fascia lata and are therefore not the relevant medial and lateral boundaries for superficial dissection.
- Position: involved thigh slightly abducted and externally rotated (frog-leg) with cushioned support under the flexed knee.
- Preparation and draping should be done to expose the umbilicus, pubic tubercle, anterior superior iliac spine, and anterior thigh. 16-Fr Foley catheter is inserted into the bladder.
- Incision: oblique incision ≈2-3 cm below and parallel to the inguinal ligament (groin crease). Lateral end of incision is to a line drawn from the anterior superior iliac spine extending inferiorly and the medial end of the incision is to a line drawn from the pubic tubercle extending inferiorly
- The inguinofemoral dissection is designed to cover an area outlined superiorly by a line drawn from the superior margin of the external ring to the anterior superior iliac spine, laterally by a line drawn from the anterior superior iliac spine extending 20 cm inferiorly, and medially by a line drawn from the pubic tubercle 15 cm down the medial thigh.
- If an area of the skin overlying the cancer-bearing nodes is invaded or adherent and requires excision, an elliptical incision is made around the involved skin and then extended medially and laterally.
- In this setting, the incision may alternatively be extended superiorly from the lateral border of the ellipse and inferiorly from the medial border to make a single S-shaped incision for the iliac and inguinofemoral dissections
- Develop superior and inferior skin flaps in the plane just below the Camper's fascia.
- Camper’s fascia can be preserved and left attached to the overlying skin when the superior and inferior skin flaps are fashioned.
- Lymphatic drainage of the penis to the groin runs beneath the Camper fascia
- Superior skin and subcutaneous tissue flap is developed ≈8 cm superiorly
- Inferior skin and subcutaneous tissue flap is developed ≈6 cm inferiorly
- Care should be taken to preserve the superficial blood supply to the flaps, thus minimizing the risk of postoperative skin necrosis, infection, and wound breakdown.
- Handle the skin flap edges gently
- Consider covering skin flap edges with saline-moistened sponges
- Avoid grasping of the flap edges with forceps because this could potentially crush and devascularize the tissue.
- Camper’s fascia can be preserved and left attached to the overlying skin when the superior and inferior skin flaps are fashioned.
- Superficial lymph node dissection
- Develop a plane below Scarpa fascia
- Superior boundary: dissect the fat and areolar tissues from the external oblique aponeurosis and the spermatic cord to the inferior border of the inguinal ligament
- Inferior boundary: inferior angle of the inguinofemoral exposure at the apex of the femoral triangle
- At the inferior boundary, the Great saphenous vein is identified
- In traditional standard radical inguinal lymphadenectomy, the Great saphenous vein is ligated and divided. However, this increases the risk of lower-extremity complications and in patients with minimal metastatic disease, it may be feasible and beneficial to spare the saphenous vein.
- In modified inguinal lymphadenectomy (see below), the Great saphenous vein is spared.
- At the inferior boundary, the Great saphenous vein is identified
- Deep lymph node dissection
- Incise fascia lata just below the inguinal ligament, along its lateral margin
- Continue dissection down through the fascia lata overlying the sartorius muscle laterally and the thinner fascia covering the adductor longus muscle medially.
- Use both blunt and sharp dissection to resect the deep inguinal nodes.
- Use clips for meticulous control of lymphatic channels to avoid a lymphatic leak.
- At the apex of the femoral triangle, the femoral artery and vein are identified.
- The anterior aspects of the femoral vessels are dissected, but the femoral vessels are not skeletonized, and the lateral surface of the femoral artery is not exposed.
- This avoids injury to the femoral nerve and the deep femoral artery
- The femoral nerve is usually not visible as it runs beneath the iliacus fascia lateral to the femoral artery.
- This avoids injury to the femoral nerve and the deep femoral artery
- The anterior aspects of the femoral vessels are dissected, but the femoral vessels are not skeletonized, and the lateral surface of the femoral artery is not exposed.
- In standard radical inguinal lymphadenectomy, the saphenous vein is divided at the saphenofemoral junction
- Dissection is continued superiorly along the femoral vessels to include the deep inguinal nodes, working medially to laterally over the femoral vein and artery until the femoral canal is reached.
- Superficial cutaneous perforating arteries are ligated as they are encountered on the surface of the femoral artery.
- Coverage over the femoral vessels and nerves: if needed, the sartorius muscle can be transposed as rotational flap by releasing its attachments from the ASIS, providing myocutaneous coverage over the femoral vessels and nerves
- The sartorius flap is sutured to the inguinal ligament superiorly with interrupted 2-0 Vicryl sutures, and its margins are sutured to the muscles of the thigh immediately adjacent to the femoral vessels
- Closure
- Primary closure of the inguinofemoral dissection is usually possible with minimal or no further mobilization of the excision margins.
- When circumstances demand a large area of inguinal soft tissue sacrifice, primary closure may be obtained by scrotal skin rotation flaps an abdominal wall advancement flap or a myocutaneous flap based on the rectus abdominis or tensor fasciae latae for more extensive defects.
- Closed-suction drains are placed under the subcutaneous tissue and brought out inferiorly, to prevent lymphocele formation.
- The wound is subsequently closed in multiple layers with 2-0 and 3-0 Vicryl sutures.
- During closure, the skin flaps are sutured to the surface of the exposed musculature to decrease dead space.
- This can minimize the risk of a postoperative fluid collection (i.e., seroma) that may serve as a potential source for infection.
- During closure, the skin flaps are sutured to the surface of the exposed musculature to decrease dead space.
- The skin is closed with 3-0 Monocryl or staples.
- Primary closure of the inguinofemoral dissection is usually possible with minimal or no further mobilization of the excision margins.
- Post-operative care
- Ambulation is strongly advised immediately after surgery
- Bed rest for 2 or 3 days is only used if myocutaneous or other large skin flap is used.
- Efforts to minimize lymphedema during the initial postoperative period include applying thigh-high elastic wraps or stockings and elevating the foot of the bed.
- Closed-suction rains are removed after when drainage is less than 30-50 mL/day for consecutive shifts.
- A suppressive dose of a cephalosporin for 1 to 2 months may be used until healed to decrease the incidence of erythema and cellulitis, and this seems to improve overall wound healing.
- Ambulation is strongly advised immediately after surgery
- Boundaries of dissection:§
Adverse events[edit | edit source]
- Hemorrhage
- Seroma or lymphocele
- Lymphedema, debilitating lymphedema
- Wound infection ornecrosis
- Flap necrosis
- DVT
- Sepsis
- Strong risk factor for complications is palliative indication for ILND§
Modified complete inguinal lymphadenectomy[edit | edit source]
- Less morbidity than standard radical inguinal lymphadenectomy
- Key aspects of the procedure are (5):
- Shorter skin incision
- Limiting dissection by excluding the area lateral to the saphenous vein and femoral vein§
- Lateral limit of dissection saphenous and femoral vein in modified dissection, compared to sartorius muscle in standard inguinal lymphadenectomy
- Preservation of the saphenous vein
- Elimination of the need to transpose the sartorius muscle
- Thicker skin flaps
Technique[edit | edit source]
- Position as above
- Incision: 10-cm skin incision is made ≈1.5-2 cm below the inguinal crease
- Skin flaps are developed in the plane just beneath the Scarpa fascia for a distance of 8 cm superiorly and 6 cm inferiorly.
- The superior dissection is carried to the level of the external oblique fascia with exposure of the spermatic cord. A funiculus of lymphofatty tissue, extending from the base of the penis to the superomedial portion of the lymph node packet, is ligated and divided.
- Dissection commences in a caudad direction with removal of the superficial and deep inguinal nodes
- The saphenous vein is identified and preserved, although a number of branches draining into it will need to be sacrificed.
- The nodal packet is dissected caudad to the level of the skin flap dissection, at which point the lymphatics are carefully ligated and the specimen is delivered from the operative field
- A closed-suction drain is placed, and the incision is closed in standard fashion
Adverse events[edit | edit source]
- Primarily minor
- Seroma or lymphocele (0-26%)
- Lymphorrhea (9-10%)
- Wound infection and skin necrosis (0-15%)
Endoscopic and robotic inguinal lymphadenectomy[edit | edit source]
- The morbidity of an endoscopic inguinal lymph node dissection is lower than previously reported for open contemporary series with a similar number of nodes being harvested
Questions[edit | edit source]
- What part of the penis is drained by the superficial vs. deep lymphatic system?
- Which lymph nodes do the superficial vs. deep lymphatics of the penis drain to?
Answers[edit | edit source]
- What part of the penis is drained by the superficial vs. deep lymphatic system?
- Which lymph nodes do the superficial vs. deep lymphatics of the penis drain to?
References[edit | edit source]
- Hinman’s Atlas of Urologic Surgery, 4th Edition Joseph A. Smith, Jr., Stuart S. Howards, Glenn M. Preminger, Roger R. Dmochowski
- Wein AJ, Kavoussi LR, Partin AW, Peters CA (eds): CAMPBELL-WALSH UROLOGY, ed 11. Philadelphia, Elsevier, 2015, vol 1, chap 39
- Leone, Andrew, et al. "Contemporary management of patients with penile cancer and lymph node metastasis." Nature Reviews Urology 14.6 (2017): 335-347.