Hypercortisolism
Jump to navigation
Jump to search
Hypothalamus-Pituitary-Adrenal (HPA) Axis[edit | edit source]
- Hypothalamus
- Produces corticotropin-releasing hormone (CRH)
- Corticotropin-releasing hormone (CRH)
- Function:
- Acts on the corticotropic cells of the anterior pituitary to make ACTH
- Secretion
- Under tight control of the hypothalamic suprachiasmatic nucleus
- Follows circadian patterns.
- The highest level of cortisol in healthy subjects is detected in the mornings, and the nadir is observed at approximately 11 PM.
- Even small perturbations of this physiologic rhythm are considered pathologic
- The highest level of cortisol in healthy subjects is detected in the mornings, and the nadir is observed at approximately 11 PM.
- Function:
- ACTH
- Functions (2):
- Stimulates production of glucocorticoids and androgens by the adrenal cortex
- Plays a critical role in maintaining adrenal cortical vitality.
- Without ACTH (e.g., when its secretion is suppressed by exogenous steroid intake), all but the mineralocorticoid(aldosterone)-producing cells of the adrenal cortex atrophy
- Secretion:
- Stimulated by (3):
- CRH (most important)
- Oxytocin
- Vasopressin
- Stimulated by (3):
- Functions (2):
- Glucocorticoids act on to the hypothalamus and pituitary to inhibit production of CRH and ACTH (negative feedback)
- Patients with hypercortisolism may be at higher risk for post-adrenalectomy adrenal insufficiency than patients with non-cortisol secreting adrenal pathologies, because functionality of the contralateral gland may be suppressed
- Stress, whether physiologic or psychologic, appears to be the most important variable in modulating activity of the HPA axis
Pathophysiology[edit | edit source]
- Definition of Cushing's syndrome: hypercortisolism secondary to excessive production of glucocorticoids by the adrenal cortex
- Causes of Cushing's syndrome
- Categorized into 3 main groups: exogenous vs. ACTH-dependent vs. ACTH-independent
- Exogenous
- Most common cause of hypercortisolism in patients of the Western world
- Can cause virilization, including hirsutism, but should not elevate ketosteroid levels
- ACTH-dependent (endogenous)
- 85% of cases of endogenous Cushing syndrome
- Results from an increased serum ACTH level
- Caused by pathology extrinsic to the adrenal gland:
- Primary pituitary pathology (also known as Cushing disease)
- Most common (80%) cause of ACTH-dependent hypercortisolism
- Ectopic ACTH production
- Nearly always malignant; the most common associated malignancies are bronchial carcinoid, small cell lung cancer, and less often pheochromocytoma
- Ectopic CRH syndrome
- Extremely uncommon; bronchial carcinoma is the most common cause
- Primary pituitary pathology (also known as Cushing disease)
- ACTH-independent (endogenous)
- 15% of cases of endogenous Cushing syndrome; relatively rare
- Cause by pathology intrinsic to the adrenal gland
- Results from unregulated overproduction of glucocorticoids by the adrenal(s), either unilateral neoplasm or rarely, bilateral disease
- Exogenous
- Categorized into 3 main groups: exogenous vs. ACTH-dependent vs. ACTH-independent
- Subclinical Cushing syndrome
- Hypercortisolemia in the absence of an overt cushingoid phenotype
- Surgical indications for subclinical Cushing syndrome are still a matter of debate.
- Some argue that adrenalectomy should be performed only in patients who are potentially symptomatic and exhibit clinical signs, such as hypertension, obesity, glucose intolerance, or osteopenia. Others argue that surgery must be offered to all patients to prevent the sequelae of hypercortisolism.
- Other conditions can stimulate the Hypothalamus-Pituitary-Adrenal axis and mimic Cushing’s syndrome
- Causes of hypercortisolism in the absence of Cushing’s syndrome:
- Some features of Cushing syndrome may be present:
- Morbid obesity
- Glucocorticoid resistance
- Poorly controlled diabetes mellitus
- Pregnancy
- Depression
- Alcohol dependence
- Unlikely to have any clinical features of Cushing syndrome
- Physical stress (hospitalization, surgery, pain)
- Malnutrition, anorexia nervosa
- Intense chronic exercise
- Hypothalamic amenorrhea
- Corticosteroid-binding globulin excess (increased serum but not in urine cortisol)
- Some features of Cushing syndrome may be present:
- Causes of hypercortisolism in the absence of Cushing’s syndrome:
Diagnosis and Evaluation[edit | edit source]
History and Physical Exam[edit | edit source]
- See Campbell's 11th edition Table 65-2 for Primary Effects of Glucocorticoids
- Classic symptoms of hypercortisolism, such as central obesity, moon facies, buffalo hump, facial plethora, menstrual disturbances, hirsuitism, proximal muscle weakness, easy bruisability, and abdominal striae, are nonspecific.
- Cushing syndrome also results in systemic symptomatology, such as dyslipidemia, insulin resistance, and hypertension, similar to the highly-prevalent metabolic syndrome
Insert image
- Urological complications of Cushing's syndrome
- Erectile dysfunction, decreased libido
- Hypogonadal hypogonadism
- Relatively common in men with Cushing syndrome
- Consider initiating a hypercortisolism workup in men with libido or erectile problems, low testosterone, and low gonadotropin levels
- Urolithiasis
- Up to 50% of patients with Cushing syndrome exhibit urolithiasis
- Stone formers with cushingoid features also should receive a hypercortisolemia evaluation
Labs[edit | edit source]
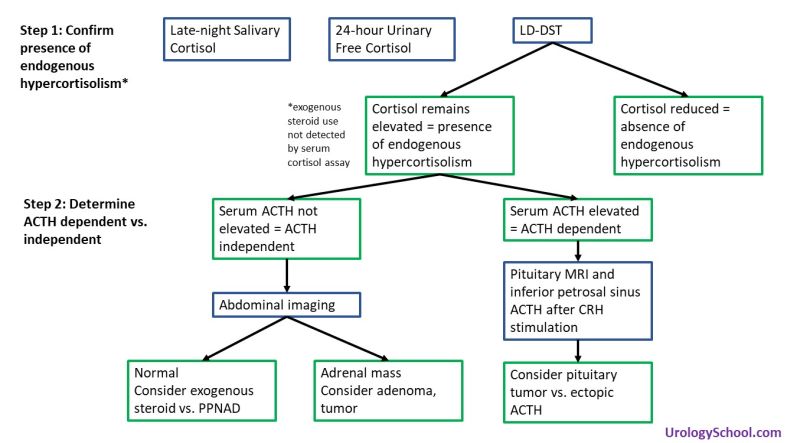
- Most frequently performed laboratory tests (3):
- Overnight low-dose dexamethasone suppression test (LD-DST) (sensitivity: 85-90, specificity: 95-99)
- Late-night salivary cortisol (sensitivity: 92-100, specificity: 93-100§)
- 24-hour urinary free cortisol (sensitivity: 80-98 specificity: 45-98)
- 2011 CUA Guidelines on Incidental Adrenal Mass recommend LD-DST
- Second-line tests:
- 2-day low-dose dexamethasone suppression test
- Midnight plasma cortisol testing
- Low-dose dexamethasone suppression test (LD-DST)
- Recommended in the evaluation of an incidental adrenal mass (2011 CUA Guidelines on Incidental Adrenal Mass)
- Determines the presence of endogenous hypercortisolism, not the cause
- To evaluate the patient’s glucocorticoid negative feedback system, a low-dose (1 mg) of dexamethasone is administered overnight followed by measurement of morning serum cortisol. The dose of dexamethasone administered is supraphysiologic and corresponds to 3-4x the level of physiologic glucocorticoids
- In patients without hypercortisolism, the dexamethasone acts on the corticotropic cells of the anterior pituitary, suppresses ACTH production, and thereby results in a reduction of serum cortisol levels.
- In patients with hypercortisolism due to endogenous causes, the dexamethasone fails to suppress cortisol production due to the relative insensitivity of pituitary adenomas to the inhibitory effects of glucocorticoid stimulation resulting in elevated serum cortisol levels despite dexamethasone.
- Exogenous steroid use cannot be ruled out with this test.
- Exogenous steroids, including that used for the test, are not detected by the serum cortisol assay.
- Pharmaceuticals That Affect Overnight Low-Dose Dexamethasone Suppression Testing for Cushing Syndrome
- Drugs that accelerate dexamethasone metabolism by induction of CYP3A4
- Phenobarbital
- Phenytoin
- Carbamazepine
- Primidone
- Rifampin
- Rifapentine
- Ethosuximide
- Pioglitazone
- Drugs that impair dexamethasone metabolism by inhibition of CYP3A4
- Aprepitant, fosaprepitant
- Itraconazole
- Ritonavir
- Fluoxetine
- Diltiazem
- Cimetidine
- Drugs that increase cortisol-binding globulin and may falsely elevate cortisol results
- Estrogens
- Mitotane
- Drugs that accelerate dexamethasone metabolism by induction of CYP3A4
- LD-DST can yield as high as a 50% false-positive rate in women using oral contraceptives
- Contraceptives increase total (but not bioavailable) cortisol levels by raising the patient’s cortisol-binding globulin concentrations
- Late night salivary cortisol and midnight plasma cortisol demonstrate a perturbation, and in some cases complete disruption, of the diurnal variation of cortisol levels
- 24-hour urinary free cortisol
- May not be sensitive for subclinical Cushing syndrome, and the Endocrine Society recommends against it for metabolic evaluation of adrenal incidentalomas
- Drugs that increase urine free cortisol results
- Carbamazepine
- Fenofibrate (increase if measured by high-performance liquid chromatography)
- Some synthetic glucocorticoids (immunoassays)
- Drugs that inhibit 11β-hydroxysteroid dehydrogenase type 2 (licorice, carbenoxolone)
- After confirming hypercortisolism, serum ACTH is measured to distinguish ACTH-independent causes from ACTH-dependent causes
- Low serum ACTH
- Suggests ACTH-independent pathology
- Abdominal imaging is indicated to identify the adrenal source.
- If the adrenals are unremarkable on imaging, exogenous steroids as a cause of Cushing syndrome, or much less commonly, primary pigmented nodular adrenocortical disease (PPNAD) should be suspected.
- In PPNAD, the adrenal glands are normal in size and exhibit black or brown cortical nodules.
- If the adrenals are unremarkable on imaging, exogenous steroids as a cause of Cushing syndrome, or much less commonly, primary pigmented nodular adrenocortical disease (PPNAD) should be suspected.
- High serum ACTH
- Suggests pituitary source (Cushing disease) or ectopic ACTH syndrome
- Can be difficult to distinguish Cushing disease from ectopic ACTH syndrome because both pituitary and ACTH-producing tumours can be very difficult to localize with imaging.
- Direct measurements of ACTH in the inferior petrosal sinus, a downstream venous plexus that drains the pituitary, after CRH stimulation has become the gold standard approach for distinguishing ectopic ACTH production from Cushing disease.
- High-dose dexamethasone suppression testing was used in the past to differentiate pituitary and ectopic ACTH sources, but the value of the test is limited.
- The study is based on the principle that high enough doses of dexamethasone should suppress ACTH production by pituitary adenomas, whereas ectopic ACTH production continues despite the high-dose glucocorticoid administration
- Low serum ACTH
Management[edit | edit source]
- ACTH-independent disease: ipsilateral adrenalectomy
- Medications that block enzymes of steroid synthesis (mitotane, metyrapone, aminoglutethimide trilostane, ketoconazole, etomidate) are used for bridging a hypercortisolism patient to surgery or when surgical intervention is not possible.
- Cushing disease (ACTH-secreting pituitary adenoma): trans-sphenoid surgical resection
- Bilateral adrenalectomy is most often recommended when at least one attempt to treat the primary tumor has failed. It is also necessary in rare instances when hypercortisolism is life-threatening and swift definitive treatment is mandatory. Lifelong mineralocorticoid and glucocorticoid replacement is required in all patients.
- Patients undergoing bilateral adrenalectomy are at risk (8-29%) for progressive growth of their pituitary adenoma, resulting in complications such as ocular chiasm compression, oculomotor deficiencies, and, rarely, a rise in intracranial pressure, resulting in the Nelson-Salassa syndrome (also known as Nelson syndrome), which is found in 8-29% of patients who have undergone bilateral adrenalectomy.
- When counseling patients regarding bilateral adrenalectomy for ACTH-dependent Cushing syndrome, the urologist must also warn of the rare possibility of residual, functioning adrenal tissue remaining after the procedure
- Bilateral adrenalectomy is most often recommended when at least one attempt to treat the primary tumor has failed. It is also necessary in rare instances when hypercortisolism is life-threatening and swift definitive treatment is mandatory. Lifelong mineralocorticoid and glucocorticoid replacement is required in all patients.
- Ectopic ACTH production: resection of the ACTH-producing tumor.
- Primary tumor resection is possible in only 10% of patients.
- For patients with unresectable primary tumors or whose primary ACTH-producing tissue cannot be identified, bilateral adrenalectomy with lifelong replacement therapy is an excellent therapeutic option
Questions[edit | edit source]
- What is the role of ACTH? Where is ACTH secreted from? What stimulates release of ACTH?
- How are the causes of hypercortisolism/Cushing’s syndrome categorized? Which is the most common cause in the Western world? Which does Cushing’s disease fall under?
- What are clinical manifestations of hypercortisolism?
- What are non-adrenal urologic manifestations of hypercortisolism?
- What is subclinical Cushing’s syndrome?
- What non-radiographic tests can be used to detect Cushing’s syndrome?
- Which form of hypercortisolism cannot be evaluated with the low-dose dexamethasone suppression test?
- After confirming hypercortisolism, how can you distinguish ACTH-dependent from ACTH-independent causes?
- List causes of hypercortisolism other than Cushing’s syndrome.
Answers[edit | edit source]
- What is the role of ACTH? Where is ACTH secreted from? What stimulates release of ACTH?
- Stimulate production of glucocorticoids and sex hormones
- Anterior pituitary
- CRH from the hypothalamus
- How are the causes of hypercortisolism/Cushing’s syndrome categorized? Which is the most common cause in the Western world? Which does Cushing’s disease fall under?
- Exogenous vs. Endogenous. Endogenous classified as ACTH-dependant vs. ACTH-independent
- Exogenous most common cause in Western world
- Cushing’s disease is an ACTH-dependant cause
- What are clinical manifestations of hypercortisolism?
- Central obesity, moon facies, buffalo hump, facial plethora, erectile dysfunction, decreased libido, menstrual disturbances, hirsuitism, proximal muscle weakness, easy bruisability, and abdominal striae
- What are non-adrenal urologic manifestations of hypercortisolism?
- Hypogonadal hypogonadism (negative feedback from glucocorticoids on pituitary and hypothalamus) and urolithiasis
- What is subclinical Cushing’s syndrome?
- Hypercortisolemia without overt clinical manifestations
- What non-radiographic tests can be used to detect Cushing’s syndrome?
- Low-dose desamethasone suppression test
- Late night salivary cortisol
- 24 hour urinary cortisol
- Which form of hypercortisolism cannot be evaluated with the low-dose dexamethasone suppression test?
- After confirming hypercortisolism, how can you distinguish ACTH-dependent from ACTH-independent causes?
- Serum ACTH
- List causes of hypercortisolism other than Cushing’s syndrome.
References[edit | edit source]
- Wein AJ, Kavoussi LR, Partin AW, Peters CA (eds): CAMPBELL-WALSH UROLOGY, ed 11. Philadelphia, Elsevier, 2015, chap 65