Functional: Urinary Fistulae
Jump to navigation
Jump to search
Background[edit | edit source]
- Definition of fistula: an extra-anatomic communication between two or more epithelial- or mesothelial-lined body cavities or the skin surface
- Management principles
- Factors to consider in the initial approach to urinary fistula and in those patients in whom primary therapy has failed Fistula TO MIIND (8):
- Presence of a Foreign body
- Technical surgical problems
- Urinary Obstruction; remove or bypass distal urinary obstruction
- Malignancy; beware of malignant cause of fistula
- Biopsy of the fistula tract should be performed in any patient with a fistula and a prior history of malignancy
- Ischemia or Infection
- Nutrition
- Drainage; achieve unobstructed urinary drainage and/or stenting
- Principles of Surgical Repair of Urinary Fistula (11):
- Adequate exposure of the fistula tract
- Debridement of devitalized and ischemic tissue
- Removal of involved foreign bodies or synthetic materials from region of fistula, if applicable
- Careful dissection and/or anatomic separation of the involved organ cavities
- Watertight closure
- Use of well-vascularized, healthy tissue flaps for repair (atraumatic handling of tissue)
- Multiple-layer closure
- Tension-free, nonoverlapping suture lines
- Adequate urinary tract drainage and/or stenting after repair
- Treatment and prevention of infection (appropriate use of antimicrobials)
- Maintenance of hemostasis
- Factors to consider in the initial approach to urinary fistula and in those patients in whom primary therapy has failed Fistula TO MIIND (8):
Urogynecologic fistulae[edit | edit source]
Vesicovaginal fistula[edit | edit source]
- 75% of acquired urinary tract fistula are VVF
Causes[edit | edit source]
- Radical Obstetrical Colleagues’ Trauma Causes Incontinence Fistula (7):
- Radiation
- May occur several decades after completion of the radiation therapy
- Any fistula after radiation therapy for malignancy may represent a recurrence of the malignancy
- Obstetric
- Causes: obstructed labor, forceps laceration, uterine rupture, cesarean section injury to bladder
- In the developing world, where routine perinatal obstetric care may be limited, VVF most commonly occurs as a result of prolonged obstructed labor resulting from cephalopelvic disproportion, with resulting pressure necrosis to the anterior vaginal wall, bladder, bladder neck, and proximal urethra from the baby.
- Typically, these occur in individuals who are young primigravidas with a narrow bony pelvis.
- The constellation of problems resulting from obstructed labor is not limited to VVF and has been termed the obstructed labor injury complex.
- In the developing world, where routine perinatal obstetric care may be limited, VVF most commonly occurs as a result of prolonged obstructed labor resulting from cephalopelvic disproportion, with resulting pressure necrosis to the anterior vaginal wall, bladder, bladder neck, and proximal urethra from the baby.
- Obstetric fistulae are more likely to be:
- Larger
- Located distally in the vagina
- Involve large portions of the bladder neck and proximal urethra
- Because of their size and extensive ischemia of the surrounding tissues, these fistulae are often difficult to repair.
- Causes: obstructed labor, forceps laceration, uterine rupture, cesarean section injury to bladder
- Cancer
- Trauma
- Postsurgical: abdominal hysterectomy, vaginal hysterectomy, anti-incontinence surgery, anterior vaginal wall prolapse surgery (e.g., colporrhaphy), vaginal biopsy, bladder biopsy, endoscopic bladder resection, laser therapy in bladder, other pelvic surgery (e.g., vascular, rectal)
- In the industrialized world, the most common cause (>75%) is injury to the bladder at the time of surgery, the most common of which is hysterectomy
- The rate of iatrogenic bladder injury during abdominal hysterectomy is ≈0.5-1.0%; the rate of incidence of fistula after hysterectomy is ≈0.1-0.2%.
- Post-hysterectomy VVFs are thought to result most commonly from an incidental unrecognized iatrogenic cystotomy near the vaginal cuff.
- If unrecognized intraoperatively, a pelvic urinoma may develop and ultimately drain out through the vaginal cuff. Ongoing urinary drainage along this tract results in a fistula.
- Other potential mechanisms for post-hysterectomy VVF include tissue necrosis from:
- Cautery
- A suture placed through both the bladder and vaginal wall during closure of the vaginal cuff
- An attempt to control pelvic bleeding by suture ligature
- Tissue ischemia and then necrosis promotes fibrosis and induration, finally resulting in an epithelial or mucosal lining of the tract and the development of a fistula tract.
- Clear vaginal discharge after hysterectomy does not invariably represent a urinary fistula or incontinence. Other than normal vaginal secretions, less common causes include a peritoneovaginal fistula, lymphatic fistula, vaginitis, and fallopian tube fluid
- In the industrialized world, the most common cause (>75%) is injury to the bladder at the time of surgery, the most common of which is hysterectomy
- External trauma (e.g., penetrating, pelvic fracture, sexual)
- Postsurgical: abdominal hysterectomy, vaginal hysterectomy, anti-incontinence surgery, anterior vaginal wall prolapse surgery (e.g., colporrhaphy), vaginal biopsy, bladder biopsy, endoscopic bladder resection, laser therapy in bladder, other pelvic surgery (e.g., vascular, rectal)
- Congenital
- Infectious or Inflammatory cause
- Foreign body (vaginal mesh for prolapse repair)
- Radiation
Differential Diagnosis[edit | edit source]
- Other causes of urinary incontinence, including SUI, urge (bladder) incontinence, and overflow incontinence, as well as ureterovaginal fistula.
Diagnosis and Evaluation[edit | edit source]
UrologySchool.com Summary[edit | edit source]
- Recommended (4)
- History and Physical Exam
- Labs
- Urinalysis +/- culture
- Imaging:
- Lower tract imaging (with cystogram and/or voiding cystourethrogram (VCUG))
- Upper tract imaging (with CT urography)
- Other
- Cystoscopy
- Optional
- Dye test
Recommended[edit | edit source]
- History and Physical Exam
- History
- Most common complaint is constant urinary drainage per vagina
- The amount of urinary leakage can vary considerably from patient to patient and may be proportional to the size of the fistula tract.
- Pain is uncommon
- Most common complaint is constant urinary drainage per vagina
- Physical exam
- A pelvic examination with a speculum should always be performed.
- VVFs after hysterectomy are most commonly located along the anterior vaginal wall at the level of the vaginal cuff
- Visual and manual assessment of inflammation surrounding the fistula is necessary, because it may affect timing of the repair.
- Significant inflammation, infection, or induration around the fistula may mitigate against immediate repair.
- A pelvic examination with a speculum should always be performed.
- History
- Laboratory
- Urinalysis +/- culture, when indicated
- Cytology, when indicated
- Imaging
- Lower tract imaging (with cystogram and/or voiding cystourethrogram (VCUG))
- A cystogram that fails to demonstrate a suspected VVF but lacks voiding images or postvoid images should be considered non-diagnostic.
- Upper tract imaging (with CT urography)
- Up to 12% of postsurgical VVFs have an associated ureteral injury or ureterovaginal fistula
- Lower tract imaging (with cystogram and/or voiding cystourethrogram (VCUG))
- Other
- Cystoscopy
- Should be performed in patients for whom a suspicion of VVF is present
- Cystoscopy
Optional[edit | edit source]
- Dye test
- The presence of a VVF may be confirmed by instilling a colored solution, such as methylene blue or indigo carmine into the bladder per urethra and observing whether vaginal drainage is discolored
- Small or occult fistulae may be identified in this fashion.
- Staining at the introital (distal) end of the packing suggests urinary incontinence or a urethrovaginal fistula, whereas proximal staining suggests a VVF
- If the vaginal packing remains dye-free with this maneuver, then the possibility of a ureterovaginal fistula can be investigated with the use of clean vaginal packing, IV indigo carmine (or other vital dye), and a repeat pad test. Blue staining at the proximal end of the pad after this maneuver suggests the presence of a ureterovaginal fistula
- A double dye or tampon test may confirm the diagnosis of urinary fistula, as well as suggesting the possibility of an associated ureterovaginal or urethrovaginal fistula. In one variation of the double dye test, a tampon is placed per vagina. Oral phenazopyridine is administered, and vital blue dye is instilled into the bladder. If the tampon is discolored
- Yellow-orange at the top, it is suggestive of a ureterovaginal fistula
- Green (a combination of blue and yellow) discoloration in the midportion of the tampon suggests VVF
- Blue staining at the bottom suggests a urethrovaginal fistula
- The presence of a VVF may be confirmed by instilling a colored solution, such as methylene blue or indigo carmine into the bladder per urethra and observing whether vaginal drainage is discolored
Management[edit | edit source]
- Options (3):
- Indwelling catheter
- Fulguration
- Fibrin sealant
- Surgery
Indwelling catheter[edit | edit source]
- A trial of indwelling catheterization and anticholinergic medication for at least 2-3 weeks may be warranted in selected patients with newly diagnosed VVF, because spontaneous healing may result (spontaneous closure rate ≈13%)
- Drainage of the bladder should start immediately to prevent epithelialization of the fistula tract.
- Characteristics associated with favorable outcomes
- Size <2-3 mm
- Simple injuries to the bladder that do not involve devascularization or thermal injury spread that result in interrupted blood supply to the area
- Fistulous tracts that remain open ≥3 weeks after adequate catheter drainage are unlikely to resolve without further intervention
Fulguration[edit | edit source]
- Patients with small epithelialized fistulae, usually <3-5 mm in diameter, may benefit from a minimally invasive treatment involving disruption of the epithelial layer of the fistula tract.
- A small cautery electrode is passed into the fistula tract endoscopically as far as possible. The electrode is slowly withdrawn from the tract with the electrode set on coagulation.
- Catheterization may be combined with minimally invasive electrocoagulation of the fistula tract.
- Fulguration risks failure and the possibility of enlarging the size of the fistula in patients with:
- Thin vesicovaginal septum
- Large VVF
- Non-oblique fistula tract
- Significant inflammation around the fistula tract.
Fibrin sealant[edit | edit source]
- Has been used as an adjunctive measure to treat VVF
Surgery[edit | edit source]
- Pre-operative Counselling
- Sexual activity should be documented
- Some vaginal procedures, including the Latzko procedure, may result in vaginal shortening and postoperative dyspareunia
- Pre-operative estrogen supplementation may be beneficial in the postmenopausal patient with vaginal atrophy; topical estrogen preparations may improve vascularity and local tissue quality
- Sexual activity should be documented
- Technique
- Approaches (2):
- Transvaginal
- Transabdominal (transvesical)
- Success rates are similar between the two approaches
- The most important factor is the experience of the operating surgeon
- Advantages of transvaginal approach (3):
- Shorter operative times
- Shorter hospital stay
- Less blood loss
- Disadvantages of transvaginal approach (3):
- Relative lack of familiarity of the vaginal cuff anatomy to many urologists
- Potential for vaginal shortening, especially with the Latzko approach
- Difficulty in exposing high or retracted fistulae located near the vaginal cuff, especially in deep, narrow vaginas, or in those without any apical prolapse (though these are not contraindications)
- Advantages of abdominal approach (2):
- Other intra-abdominal pathology requiring repair
- Complicated fistulae including those associated with multiple prior failed attempts at repair, or those that are large (>5cm)
- No difference in risk of ureteral injury in transabdominal vs. transvaginal approach
- Success rates are similar between the two approaches
- Excision of the fistula tract itself is not always necessary and may even compromise the repair in some patients
- Transvaginal approach to VVF repair uses a 3-4 layer closure
- Tissue interposition
- The interposition of a healthy, well-vascularized tissue flap during VVF repair may be beneficial under certain circumstances, such as (6):
- Recurred after a prior attempt at repair
- Related to previous radiotherapy
- Ischemic or obstetric fistulae
- Large fistulae
- Associated with a difficult or tenuous closure because of poor tissue quality
- Most commonly used flaps for VVF repaired:
- Transvaginal repair: Martius flap or peritoneum
- Transabdominal: omentum or peritoneum
- Other options for a flap include:
- Gracilis muscle
- Labial myocutaneous flaps
- Seromuscular intestinal flaps
- Rectum abdominis flaps
- Martius flap
- Labial fat pad consisting of adipose tissue and connective tissue
- Blood supply derives from (3):
- Superiorly from the external pudendal artery
- Laterally from the obturator artery
- Inferiorly from the posterior labial vessels (branch of the internal pudendal artery)
- Preferred for low or distal fistulae involving the trigone, bladder neck, and urethra
- Peritoneal flap
- Preferred for high-lying post-hysterectomy VVF
- For post-hysterectomy fistulae, the distance from the labial harvesting site of the Martius flap to the fistula at the apex of the vagina may be considerable. Mobilizing and then tunneling the Martius flap to reach this location may compromise its blood supply and viability.
- May also be used as an adjunctive measure during transabdominal repair of VVF, although the approach and technique are vastly different
- Preferred for high-lying post-hysterectomy VVF
- Omental flap
- Blood supply derives from right and left gastroepiploic arteries
- Blood supply enters the omentum perpendicular to its origin off the greater curvature of the stomach, enabling vertical incisions and mobilization into the deep pelvis.
- In many individuals the flap will reach into the deep pelvis without mobilization and without tension; however, wide mobilization may be necessary to permit the omentum to reach the deep pelvis in some cases; however,
- Can be a useful adjunctive measure in the setting of infection or inflammation because of its rich blood supply and lymphatic properties
- Blood supply derives from right and left gastroepiploic arteries
- Martius flap
- The interposition of a healthy, well-vascularized tissue flap during VVF repair may be beneficial under certain circumstances, such as (6):
- Postoperative drainage
- Can be maintained by single or dual catheters.
- Most commonly, both urethral and suprapubic drainage catheters are left postoperatively; the disadvantage to single-catheter drainage is principally that the catheter will malfunction, clog, or kink, resulting in bladder filling, eventual overdistention, and disruption of the suture line.
- Can be maintained by single or dual catheters.
- Timing of repair
- Timing of repair is somewhat controversial
- Radiation-induced fistula should be repaired after the fistula has matured
- Approaches (2):
- Complications
- Late post-operative (3):
- Vaginal shortening
- Vaginal stenosis
- Recurrence of the fistula
- Late post-operative (3):
- Follow-up
- A postoperative cystogram should include voiding or postvoiding images to ensure that the VVF has been adequately repaired
- There is no standard filling volume for cystography.
- Generally, 2 to 3 weeks from surgery is an adequate time period for postoperative imaging.
- A postoperative cystogram should include voiding or postvoiding images to ensure that the VVF has been adequately repaired
- The success rate reported for a simple VVF repair is >90%.
- Complicated VVFs, including those resulting from obstetric causes, larger fistulae, and those associated with radiation, generally have a lower success rate.
- Radiation-induced fistulae can be repaired vaginally, and adjuvant flaps are used to bolster the repair
- In patients with obstetric fistulae associated with loss of the bladder neck and proximal urethra, relatively high rates of persistent severe sphincteric incontinence are noted despite successful repair of the VVF
- Stress urinary incontinence may coexist with VVF; however, it is usually not related to the repair.
- Complicated VVFs, including those resulting from obstetric causes, larger fistulae, and those associated with radiation, generally have a lower success rate.
- In some patients, repair of VVF is not possible or multiple surgical attempts have failed. Urinary diversion can be considered.
- Fistulae in patients who are not candidates for surgical intervention may be managed by percutaneous ureteral occlusion and permanent nephrostomy.
Ureterovaginal fistula[edit | edit source]
Causes[edit | edit source]
- Surgical injury to the distal 1/3 ureter (below the level of the iliac vessels)
- Most common cause: hysterectomy for benign indications
- Most common injury to the urinary tract during hysterectomy is a bladder laceration.
- Although ureteral injuries are not uncommon, they occur far less frequently than bladder injuries.
- Most common injury to the urinary tract during hysterectomy is a bladder laceration.
- The pelvic ureter is intimately related to the female genital tract throughout its course.
- In the deep pelvis, the ureter passes at the lateral edge of the uterosacral ligament and ventral to the uterine artery, and then passes just lateral to the cervix and fornix of the vagina.
- In females who undergo vaginal surgery (such as hysterectomy) or sustain penetrating pelvic trauma involving the vagina, an initially unrecognized ureteral injury can present in a delayed manner with ureterovaginal fistula.
- Most common cause: hysterectomy for benign indications
- Other risk factors include: gynecologic surgery (cesarean section, anterior colporrhaphy (cystocele repair)), vascular surgery, urologic surgery including retropubic bladder neck suspensions, colon surgery, locally advanced malignancy, radiation therapy, pelvic trauma, chronic inflammatory diseases (e.g., actinomycosis), endometriosis and obesity
- Incidence of iatrogenic ureteral injury during major gynecologic surgery ≈0.5-2.5%
Diagnosis and Evaluation[edit | edit source]
- History and Physical Exam
- Most common presenting symptom is the onset of constant urinary incontinence 1-4 weeks after surgery.
- In direct contrast to VVF, in the setting of continuous urine leakage from a ureterovaginal fistula, patients will continue to report normal voiding habits because bladder filling is maintained from the contralateral, presumably undamaged, upper urinary tract
- Imaging
- Suspicion of a ureterovaginal fistula should prompt upper tract imaging
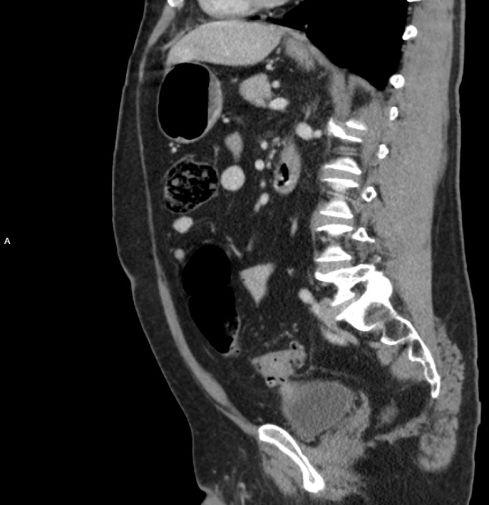
- Ureterovaginal fistulae may be seen on CT urography or MRI.
- CT urogram most commonly will demonstrate some degree of ureteral obstruction and associated caliectasis or ureteral dilation. These findings in the presence of constant vaginal drainage strongly suggest a ureterovaginal fistula.
- Alternatively, if the fistula is mature and large, the upper urinary tract may appear completely unremarkable; however, urine will be seen opacifying the vagina before the postvoid image.
- If retrograde pyelography demonstrates the fistula, as well as ureteral continuity, then an attempt at stenting is warranted.
- Cystography is performed primarily to exclude a coexistent VVF.
- A cystogram will not demonstrate the ureterovaginal fistula unless there is preexisting vesicoureteral reflux.
- Suspicion of a ureterovaginal fistula should prompt upper tract imaging
Management[edit | edit source]
- Goals of treatments are:
- Resolving urinary leakage
- Avoiding urosepsis
- Preserving of renal function
- Once the diagnosis is made, prompt drainage of the affected upper urinary tract is essential because partial ureteral obstruction is often present.
- An attempt at ureteral stenting or percutaneous nephrostomy tube decompression is warranted as soon as possible if direct open surgical repair is not immediately considered.
- Ureteral stenting may be sufficient to promote closure of the fistula in some cases
- In some cases, an antegrade stent placement will be successful where a retrograde attempt had failed.
- If ureteral stenting is unsuccessful owing to complete ureteral occlusion or if prolonged leakage persists despite stenting, then formal surgical repair is indicated
- Timing of the repair of ureterovaginal fistulae is controversial.
- Open surgical repair most commonly involves ureteroneocystostomy since most injuries occur to the distal ureter
- Repair is successful in >90% of cases
Vesicouterine fistula[edit | edit source]
- Among the least common urogynecologic fistulae
Causes[edit | edit source]
- Most common cause: Cesarean section
- Simultaneous injury to the bladder and uterus is the enticing event
Diagnosis and Evaluation[edit | edit source]
- History and Physical Exam
- Unlike other types of urogynecologic fistulae, vesicouterine fistulae may or may not manifest with constant urinary incontinence because of the sphincter-like activity of the cervix:
- Exception is in the setting of an incompetent cervix (e.g. post-partum period) wherein urinary leakage is constant
- Unlike other types of urogynecologic fistulae, vesicouterine fistulae may or may not manifest with constant urinary incontinence because of the sphincter-like activity of the cervix:
- Imaging
- Radiographic studies
- Other
- Cystoscopy
Management[edit | edit source]
- Prolonged indwelling bladder catheterization or fulguration of the fistula tract followed by bladder drainage may be successful in select cases, especially in patients with small, immature fistulae.
- Hormonal induction of menopause will induce involution of the puerperal uterus, and this principle has been used with some success in treating this condition.
- Surgical therapy for vesicouterine fistulae is often contingent on the specific reproductive wishes of the patient. If there is no further desire for childbearing, then transabdominal hysterectomy and bladder closure should be considered. For the patient who desires preservation of fertility, uterine-sparing surgery can be considered
Urethrovaginal fistula[edit | edit source]
Causes[edit | edit source]
- In industrialized countries, urethrovaginal fistulae in adults mostly have an iatrogenic cause.
- Hysterectomy is not associated with formation of urethrovaginal fistula.
- In the developing world, urethrovaginal fistula may occur as a result of obstructed labor with or without associated VVF.
Diagnosis and Evaluation[edit | edit source]
- Symptoms of urethrovaginal fistulae are largely dependent on the size and location of the fistula along the urethral lumen
- Proximal fistulae can be associated with stress incontinence, or, if they are located at the bladder neck, continuous incontinence may result, similar to that associated with VVF
- Distal fistulae beyond the sphincteric mechanism may be completely asymptomatic or may be associated with a splayed urinary stream.
- Can often be made on physical examination and cystourethroscopy; however, VCUG is most useful
- An associated VVF will be found in up to 20% of cases, and therefore a thorough evaluation of the entire lower urinary tract is warranted
Management[edit | edit source]
- Foreign material should be excised as widely as possible from the margins of the fistula
- Various types of soft-tissue flaps are often an important component of a successful urethrovaginal fistula repair including, most commonly, a Martius labial fat flap, but also gracilis and rectus abdominis muscle
- SUI may persist after repair of urethrovaginal fistulae. Whether repair of SUI should be done concomitantly with the fistula surgery or should be deferred until after repair of the fistula is controversial
Uroenteric fistula[edit | edit source]
Vesicoenteric fistula[edit | edit source]
Causes[edit | edit source]
- Diverticulitis (most common cause of colovesical fistulae)
- Malignancy (e.g. colon cancer)
- Crohn disease
- Less common causes include radiation, infection, and trauma—external penetrating trauma, as well as iatrogenic surgical trauma
Diagnosis and Evaluation[edit | edit source]
- History and physical exam
- Pneumaturia is the most common presenting symptom
- Classic presentation of vesicoenteric fistula (described as Gouverneur syndrome) consists of (4):
- Suprapubic pain
- Urinary frequency
- Dysuria
- Tenesmus
- Symptoms of vesicoenteric fistulae may originate from the urinary or GI tract; however, in general, storage LUTS are more common at presentation.
- Recurrent UTIs or cystitis refractory to antibiotic therapy may suggest a colovesical fistula
- Imaging
- Cross-sectional imaging
- Modality of choice
- CT with contrast
- Generally considered to be the most sensitive and specific modality for the diagnosis of colovesical fistulae
- Findings on CT that are suspicious for colovesical fistulae (3):
- Bladder wall thickening adjacent to a loop of thickened colon
- Air in the bladder (in the absence of previous lower urinary manipulation)
- The presence of colonic diverticula
- Cross-sectional imaging
- Cystography and transrectal contrast studies (e.g., barium enema)
- Although commonly used are less likely to demonstrate the fistula
- Cystography and transrectal contrast studies (e.g., barium enema)
- Other
- Endoscopy
- The finding of bullous edema during cystoscopy is nonspecific; however, in the appropriate clinical setting, this can be very suggestive of a colovesical fistula.
- 80-100% of cases of colovesical fistulae have an abnormality noted on cystoscopy
- The finding of bullous edema during cystoscopy is nonspecific; however, in the appropriate clinical setting, this can be very suggestive of a colovesical fistula.
- Bourne test
- Performed after a nondiagnostic barium enema.
- The first voided urine after the barium enema is immediately centrifuged and then examined radiographically. Radiodense particles in the urine are considered a positive test result and evidence for a vesicoenteric fistula
- Activated charcoal
- Oral administration of activated charcoal, which, in the setting of a fistula, will appear in the urine as black particles
- Endoscopy
Management[edit | edit source]
- Nonoperative management
- Option in selected nontoxic, minimally symptomatic patients with nonmalignant causes with vesicoenteric fistula
- Trial of medical therapy including intravenous total parenteral nutrition, bowel rest, and antibiotics may be warranted.
- May be the preferred initial approach, especially in patients with Crohn disease, in whom the notion of immediate exploratory laparotomy and bowel resection is often discouraged because of the chronic relapsing nature of the disease
- Operative management
- Goal is to separate and close the involved organs with minimal anatomic disruption and normal long-term function of both systems.
- Both single and multistage procedures have been advocated, depending on the clinical circumstances.
- A one-stage procedure involves removal of the fistula, closure of the involved organs, and primary reanastomosis of the bowel after resection of the involved bowel segment.
- A two-stage approach advocates removal of the fistula, closure of the involved organs, and creation of a temporary proximal diverting colostomy, with a later return to the operating room for colostomy takedown once the fistula tract has been demonstrated to be closed
Ureteroenteric fistula[edit | edit source]
Causes[edit | edit source]
- Most common cause: inflammatory bowel disease (e.g. Crohn’s disease)
- Usually right-sided involving the terminal ileum
- Rarely, diverticulitis or ulcerative colitis will lead to left-sided ureteroenteric fistula.
- Usually right-sided involving the terminal ileum
- Other causes include (6):
- Trauma (external and iatrogenic)
- Urothelial carcinoma
- Radiation
- Urolithiasis
- Tuberculosis
Diagnosis and Evaluation[edit | edit source]
- History and Physical Exam
- More likely to manifest with bowel rather than urinary symptoms, unlike vesicoenteric fistulae
- Pain may also be reported in the hip, flank, or anterior thigh
- Imaging
- CT and MRI are more useful than retrograde pyelography
Management[edit | edit source]
- Involves ureterolysis and possible bowel resection.
Pyeloenteric fistulae[edit | edit source]
Causes[edit | edit source]
- Most common cause has historically been chronic inflammatory disease, such as xanthogranulomatous pyelonephritis or other infectious diseases involving the kidney or bowel. However, iatrogenic surgical trauma, especially that related to percutaneous renal surgery and percutaneous nephrolithotomy (PCNL), has been associated with an increasing number of such fistulae
- Right-sided pyeloenteric fistulae most often involve the duodenum, whereas left-sided pyeloenteric fistulae most commonly involve the descending colon
Diagnosis and Evaluation[edit | edit source]
- Majority of patients have nonspecific symptoms, including malaise, nonspecific GI symptoms, urinary frequency, flank mass, or tenderness.
Management[edit | edit source]
- A large nephrostomy tube, enteric suction or bowel rest, antibiotics, and removal of any foreign body (e.g., a stone) may be attempted. Internal stenting of the urinary tract may be pursued for maximal drainage.
- Fistulae associated with a poorly functioning kidney are best treated by primary closure of the bowel and nephrectomy.
Rectourethral fistula[edit | edit source]
Causes[edit | edit source]
- Acquired rectourethral fistula may occur in the male under a variety of clinical circumstances, including those related to prostatectomy for benign or malignant disease, cryotherapy, pelvic radiotherapy, anorectal surgery, external penetrating trauma, urethral instrumentation, locally advanced prostatic or rectal malignancy, infection (e.g., TB), ruptured prostatic abscess, or inflammatory disease (e.g., Crohn disease)
- The incidence of rectourethral fistula after radical retropubic prostatectomy is low but owing to the frequency with which the operation is performed, it is the most common cause of rectourethral fistula.
- Rectal injury during radical prostatectomy occurs in < 1-2% of patients
- The incidence of rectourethral fistula after radical retropubic prostatectomy is low but owing to the frequency with which the operation is performed, it is the most common cause of rectourethral fistula.
Diagnosis and Evaluation[edit | edit source]
- History and Physical exam
- Symptoms may include fecaluria, hematuria, UTI, nausea, vomiting, and fever
- Imaging
- Lower tract imaging
- VCUG or retrograde urethrogram usually provides a definitive diagnosis of rectourethral fistula
- Upper tract imaging should be performed in patients to exclude a related ureteral injury
- Lower tract imaging
- Other
- In patients with a history of pelvic malignancy, biopsy of the fistula is suggested to evaluate for a local recurrence of the tumour
- Cystoscopy and sigmoidoscopy visualize the fistula tract in the vast majority of cases and provide a mechanism for biopsy
- Assessment of continence and sphincteric function in patients with rectourethral fistula after radical prostatectomy
- Given the location of most rectourethral fistulas at or near the vesicourethral anastomosis and the membranous urethra, there is a risk for persistent severe stress incontinence postoperatively after rectourethral fistula repair
- In patients with a history of pelvic malignancy, biopsy of the fistula is suggested to evaluate for a local recurrence of the tumour
Management[edit | edit source]
- Most rectourethral fistula will require surgical repair, although some will close with conservative management.
- Rectourethral fistula that follows open or laparoscopic prostatectomy may heal spontaneously with catheter drainage, bowel rest, and intravenous hyperalimentation.
- In some cases, fecal diversion is necessary.
- Staged repairs might be considered in (5):
- Large fistulae
- Associated with radiation therapy
- Uncontrolled local or systemic infection
- Immunocompromised states
- Inadequate bowel preparation at the time of definitive repair
- Transrectal approaches with and without division of the anal sphincter have been described for the operative repair of rectourethral fistula.
- The York-Mason procedure is a transrectal, transsphincteric approach that has been found to be effective and to have low morbidity
Urovascular fistulae[edit | edit source]
Renovascular and pyelovascular fistulae[edit | edit source]
Causes[edit | edit source]
- Most common causes are procedures in which percutaneous renal access is required, such as PCNL. Alternatively, a long-term indwelling nephrostomy tube may lead to pyelovascular fistula formation.
Diagnosis and Evaluation[edit | edit source]
- Patients may have life-threatening hemorrhage and hypovolemic shock, or intermittent gross hematuria
- ≈75% of patients with renovascular fistulae have an abdominal bruit
Management[edit | edit source]
- Depends on the cause of the fistula and the associated clinical manifestations
- Patients with severe hemorrhage on removal of the nephrostomy tube can be temporized in some instances by replacing the tube, or, in large mature tracts, by placing a Foley catheter to tamponade the bleeding.
- In patients with ongoing bleeding, transcatheter angiographic embolization of the lacerated vessel is recommended.
- ≈70% of fistulae occurring after needle biopsy of the kidney close spontaneously within 18 months, thus, expectant management is an appropriate first step
- Fistulae due to renal cell carcinoma warrant nephrectomy
Ureterovascular fistula[edit | edit source]
Causes[edit | edit source]
- Most reported ureterovascular fistulae are ureteroiliac artery fistulae, although ureteroiliac vein fistulae have been reported as well.
- Risk factors for ureteroarterial fistulae:
- Prior history of vascular disease
- Radiation therapy and/or pelvic surgery, especially in the setting of indwelling ureteral stents.
Diagnosis and Evaluation[edit | edit source]
- Ureterovascular fistulae may manifest with microscopic hematuria, intermittent gross hematuria, or life-threatening exsanguinating hemorrhage.
Management[edit | edit source]
- In a stable patient with a suspected ureterovascular fistula, radiographic evaluation can be used for diagnostic purposes and treatment planning (reconstructive options or angiographic embolization).
- In the unstable patient, surgical intervention must be considered early, especially because radiographic evaluation may be nondiagnostic.
Other urinary tract fistulae[edit | edit source]
- Nephropleural or nephrobronchial fistulae are uncommon; may occur secondary to percutaneous access to the upper urinary tract.
- Cutaneous fistulae from the urinary tract may arise from the kidney, ureter, bladder, or urethra. For newly diagnosed urocutaneous fistulae, it is imperative to evaluate for distal urinary obstruction.
Questions[edit | edit source]
- List risk factors for recurrence of urinary fistula after definitive treatment
- What are the principles of fisula repair?
- What is the most common acquired urinary fistula?
- What are the causes of a vesicovaginal fistula? What is most common cause in developed vs. developing world?
- What investigations should be ordered in suspected VVF? Uterovaginal fistula?
- What is the most common cause of a vesicouterine fistula?
- What is the most common cause of colovesical fistula? What symptoms are associated? What is the most common symptom?
- What is the preferred imaging test in colovesical fistula? What are signs of fistula on imaging?
- What is the most common cause of ureteroeneteric fistula? Which segment of bowel is most commonly involved in ureteroeneteric fistula?
- How does the presentation of ureteroenteric fistula differ from vesicoenteric fistula?
- Which segment of bowel is most commonly involved in pyeloeneteric fistula?
- What is the most common cause of rectourethral fistula?
- Most common cause of pyelovascular fistula?
Answers[edit | edit source]
- List risk factors for recurrence of urinary fistula after definitive treatment
- What are the principles of fisula repair?
- What is the most common acquired urinary fistula?
- What are the causes of a vesicovaginal fistula? What is most common cause in developed vs. developing world?
- What investigations should be ordered in suspected VVF? Uterovaginal fistula?
- What is the most common cause of a vesicouterine fistula?
- What is the most common cause of colovesical fistula? What symptoms are associated? What is the most common symptom?
- What is the preferred imaging test in colovesical fistula? What are signs of fistula on imaging?
- What is the most common cause of ureteroeneteric fistula? Which segment of bowel is most commonly involved in ureteroeneteric fistula?
- Most common cause of ureteroenteric fistula: inflammatory bowel disease
- Most commonly involved bowel segment in ureteroenteric fistula: terminal ileum
- How does the presentation of ureteroenteric fistula differ from vesicoenteric fistula?
- Vesicoenteric fistula presents with more urinary symptoms while ureteroenteric fistula presents with more bowel symptoms
- Which segment of bowel is most commonly involved in pyeloeneteric fistula?
- What is the most common cause of rectourethral fistula?
- Most common cause of pyelovascular fistula?
References[edit | edit source]
- Wein AJ, Kavoussi LR, Partin AW, Peters CA (eds): CAMPBELL-WALSH UROLOGY, ed 11. Philadelphia, Elsevier, 2015, chap 89