Adrenal: Pheochromocytoma
Jump to navigation
Jump to search
Background[edit | edit source]
- Endocrine tumor that arises from the chromaffin cells of the adrenal gland
- ≈1/3 are familial cases
- 1-25% originate outside of the adrenal gland
- When it is found outside the adrenal gland, the tumor is called a paraganglioma.
- Extra-adrenal pheochromocytomas occur in:
- Organ of Zuckerkandl (located at bifurcation of aorta)
- Sympathetic chain
- Perivesical
- ≈5% of incidental adrenal masses will have a pheochromocytoma
- Currently, malignant pheochromocytoma can only be defined by the presence of clinical metastases.
- A number of pathologic criteria to differentiate benign from malignant disease have been proposed, but to date there is no criterion agreed on.
Pathology[edit | edit source]
- Specific histopathological finding is zellballen, which are well defined nests of polygonal cells surrounded by fibrovascular stroma.
Hereditary forms of pheochromocytoma[edit | edit source]
- In cases of VHL the risk of malignancy is low but pheochromocytoma is characterized as producing norepinephrine.
- Unlike pheochromocytomas in patients with VHL, MEN2 and NF1 predominantly produce epinephrine.
- Compared to sporadic cases, in familial syndromes, the pheochromocytomas are almost always bilateral and more frequently malignant. Clinical manifestations are similar.
| Syndrome | Clinical characteristics | Risk of pheochromocytoma | Risk of malignant disease |
| Multiple endocrine neoplasia type 2A
Insert image |
|
50% | 3% |
| Multiple endocrine neoplasia type 2B |
|
50% | 3% |
| Von Hippel-Lindau (VHL), type 2 | HIPPPEEL
|
10-20% | 5% |
| Neurofibromatosis type 1 |
|
1% | 11% |
| Familial paraganglioma syndrome type 4 | Carotid body tumors (chemodectomas)
Vagal, jugular, tympanic, abdominal, thoracic paragangliomas |
20% | 30-50% |
| Familial paraganglioma syndrome type 1 | Carotid body tumors (chemodectomas)
Vagal, jugular, tympanic, abdominal, thoracic paragangliomas |
20% | <3% |
Diagnosis and Evaluation[edit | edit source]
History and Physical Exam[edit | edit source]
- History
- Signs and Symptoms
- Classic triad (3):
- Headache
- Episodic sudden perspiration
- Tachycardia
- Other symptoms (12):§
- Anxiety
- Sweating
- Palpitations
- Abdominal pain
- Chest pain
- Pallor
- Nausea
- Dyspnea
- Tremor
- Weight loss
- Flushing
- Visual disturbance
- Can have heterogenous clinical behavior due to the variability in the amount and ratio of the different catecholamines (norepinephrine, epinephrine, dopamine) secreted:
- Norepinephrine-predominant tumours (e.g., patients with von Hippel- Lindau [VHL] syndrome) have hypertension and sweating because of norepinephrine's vasoconstricting action through the α adrenoreceptor
- Epinephrine-predominant tumours (rare, usually limited to adrenals or the organ of Zuckerkandl) have syncope or hypotensive episodes because of epinephrine’s vasodilatory action through the β2 receptor
- Agonist potency order:
- α1: epinephrine ≥ norepinephrine >> isoprenaline
- α2: epinephrine ≥ norepinephrine >> isoprenaline
- β1: isoprenaline > epinephrine = norepinephrine
- β2: isoprenaline > epinephrine >> norepinephrine
- β3: isoprenaline = norepinephrine > epinephrine
- Episodic hypertensive episodes may be triggered by events such as induction of anesthesia, labor and delivery, instrumentation and biopsy of the tumor, strenuous physical activity and consumption of tyramine rich foods, such as red wine, chocolate and cheeses.
- Another serious clinical presentation may result from catecholamine induced cardiomyopathy when patients present with congestive heart failure and cardiac arrhythmias.
- Classic triad (3):
- Signs and Symptoms
Labs[edit | edit source]
- Metanephrine/catecholamine Testing
- The enzyme phenylethanolamine-N-methyltransferase (PNMT), catalyzes the conversion of norepinephrine to epinephrine, is relatively unique to the adrenal medulla (the brain and organ of Zuckerkandl also express this enzyme).
- Localization of PNMT to the adrenal medulla explains why the gland is the primary source of systemic epinephrine, despite the presence of similar chromaffin cells elsewhere in the sympathetic nervous system
- Catecholamines (dopamine, norepinephrine, and epinephrine) are produced by pheochromocytomas in varying amounts; release of these compounds into the bloodstream is often paroxysmal
- Metanephrines are the methylated metabolites of catecholamines
- O-methylation of catecholamines is catalyzed by the COMT enzyme
- O-methylation of norepinephrine produces normetanephrine, whereas epinephrine’s methylation results in formation of metanephrine.
- Together, normetanephrine and metanephrine are known as metanephrines.
- O-methylation of catecholamines is catalyzed by the COMT enzyme
- The conversion of catecholamines to metanephrines within pheochromocytomas is an uninterepted process. As such, measurement of plasma concentration of metanephrines is much more sensitive for detecting pheochromocytomas than the measurement of rises in plasma catecholamines, which may be paroxysmal.
- In the past, measurement of both urinary and serum catecholamine levels was the mainstay for evaluation of pheochromocytoma. However, these tests had moderated sensitivity and specificity and have been largely replaced by measurements of levels of metanephrines.
- Measurement of urinary catecholamines, nevertheless, is still recommended in conjunction with urinary fractionated (see below) metanephrine testing
- Measurement of plasma fractionated metanephrines and 24-hour urinary fractionated metanephrines and catecholamines are the mainstay biochemical tests to diagnose pheochromocytoma.
- Plasma fractionated metanephrines is used primary in those with high index of suspicion with 24-hour urinary fractionated metanephrines for those with low index.
- 2011 CUA Incidental Adrenal Mass guidelines recommend screening with a 24-hour urinary fractionated metanephrines and/or catecholamines.
- 2014 [most recent as of October 2019] Endocrine Society Pheochromocytoma Guidelines recommend plasma free metanephrines or 24-hour urinary fractionated metanephrines
- 2019 AUA Update on Pheochromocytoma recommended initial screening with plasma free metanephrines. Urinary fractionated metanephrines are an alternative, with slightly lower diagnosis sensitivity.
- The term fractionated is used when the laboratory report details not only the amount of each compound type (e.g., metanephrines), but also the relative concentrations of each compound (e.g., normetanephrine and metanephrine).
- The blood sample should be drawn after placing an intravenous cannula, dimming the room lights and having the patient lay supine for 30 minutes after minimizing any pain or anxiety.
- Prior to the blood draw, patients should be counseled on avoiding caffeine for a minimum of 24 hours
- Acetaminophen can produce a false-positive result owing to cross reactivity in the [serum?] assay and should be stopped for at least 5 days before testing.
- Tricyclic antidepressants and phenoxybenzamine should also be stopped, because these have been shown to be responsible for false-positive results.
- Usual antihypertensive therapy can be continued.
- Although β-blockade can potentially result in a false-positive test result, the current recommendation is to stop the medication only on repeat testing
- The enzyme phenylethanolamine-N-methyltransferase (PNMT), catalyzes the conversion of norepinephrine to epinephrine, is relatively unique to the adrenal medulla (the brain and organ of Zuckerkandl also express this enzyme).
- Vanillylmandelic Acid (VMA) Testing
- VMA is the primary end metabolite of catecholamines
- The sympathetic nervous system lacks the ability to produce epinephrine (lacks PNMT enzyme) and therefore contributes to the serum level of only normetanephrine (from norepinephrine) but not metanephrine (from epinephrine). Indeed, > 90% of metanephrine (an epinephrine metabolite) and some 20% or more of normetanephrine (a norepinephrine metabolite) in the bloodstream are derived from the adrenal medulla (PNMT is present in the brain and organ of Zuckerkandl). Therefore the relative rise of VMA levels, the combined total end metabolite of norepienphrine and epinephrine, in the presence of a pheochromocytoma is much less dramatic than the rise seen in the levels of metanephrines (from epinephrine), and therefore, the sensitivity of urine VMA levels is low. However, the specificity of VMA is high, especially in nonfamilial cases.
- Oral clonidine testing
- Used to distinguish suspected pheochromocytoma vs. essential hypertension in patients with minimally elevated plasma catecholamines.
- Patients with suspected pheochromocytoma usually present with elevated plasma catecholamines. However, they can rarely present with normal or mildly elevated plasma catecholamines.
- The oral clonidine test can help distinguish whether the signs and symptoms and minimally elevated plasma catecholamines are related to pheochromocytoma vs. essential hypertension, oral clonidine test.
- Patients with essential hypertension will experience a significant drop in norepinephrine due to suppression of production by the sympathetic nervous system, while those with pheochromocytoma will not.
- Used to distinguish suspected pheochromocytoma vs. essential hypertension in patients with minimally elevated plasma catecholamines.
Imaging[edit | edit source]
- 18F-FDG PET (fluorine-18 fluorodeoxyglucose positron emission tomography)
- Gold standard imaging modality for definitive staging in patients with pheochromocytoma.
- Superior test characteristics to CT, MRI, and metaiodobenzylguanidine (MIBG) scintigraphy.
- Better accuracy than 123I-MIBG in nearly all patients, especially for identification of metastatic disease.
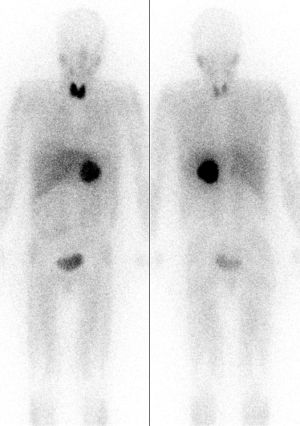 Pheochromocytoma (dark circular shadow near body center) localized by MIBG scintigraphy. See corresponding CT below. Source: Wikipedia
Pheochromocytoma (dark circular shadow near body center) localized by MIBG scintigraphy. See corresponding CT below. Source: Wikipedia
- MIBG
- Utilizes a small-molecule analog of norepinephrine
- High specificity but low sensitivity for diagnostic disease identification.
- Useful modality when a suspected pheochromocytoma cannot be localized or when metastatic disease is suspected.
- In the most common and urologically most relevant clinical scenario, a solitary adrenal mass on cross sectional imaging in the setting of a biochemical evaluation indicative of pheochromocytoma, MIBG or 18F-FDG PET may be safely be omitted because these functional studies only serve to confirm what is already known and do not alter management. However, MIBG or 18F-FDG PET imaging for large (>5 cm) tumors is likely prudent to assess for metastatic disease before surgery and thereby counsel the patient appropriately
- MRI
- Distinct low signal intensity on T1-weighted imaging
- High signal intensity on T2-weighted imaging.
- CT
- On unenhanced CT, pheochromocytomas are typically > 10 HU (mean ≈35 HU) given their rich vascularity and low lipid content. This can help differentiate them from lipid-rich adenomas
- If the lesion is not an adenoma, an adrenal mass protocol CT with IV contrast allows for evaluation of tumor washout.
- Benign adrenal lesions wash out >50% on delayed imaging while pheochromocytoma, adrenocortical carcinoma and metastatic tumors do not.
- Pheochromocytomas usually measure greater than 10 HU on unenhanced CT and >100 HU on contrast imaging, and are often well circumscribed in appearance with or without necrotic or cystic elements. Nevertheless, any evaluation of an adenoma should still include testing for plasma free metanephrines to rule out pheochromocytoma.
 CT scan with enhancement demonstrating suspicous left adrenal mass. See corresponding MIBG scan above. Source: Wikipedia
CT scan with enhancement demonstrating suspicous left adrenal mass. See corresponding MIBG scan above. Source: Wikipedia
- If the lesion is not an adenoma, an adrenal mass protocol CT with IV contrast allows for evaluation of tumor washout.
- On unenhanced CT, pheochromocytomas are typically > 10 HU (mean ≈35 HU) given their rich vascularity and low lipid content. This can help differentiate them from lipid-rich adenomas
- CT scan with enhancement demonstrating suspicious left adrenal mass. See corresponding MIBG scan above. Source: Wikipedia
Other[edit | edit source]
- Genetic counselling
- Investigation for familial syndromes is warranted in a patient younger than 50 years with a significant family history of an extraadrenal pheochromocytoma (hereditary paraganglioma syndrome), or bilateral or multifocal tumors.
- If a mutation is identified, screening should also be offered to asymptomatic at risk family members.
- Investigation for familial syndromes is warranted in a patient younger than 50 years with a significant family history of an extraadrenal pheochromocytoma (hereditary paraganglioma syndrome), or bilateral or multifocal tumors.
Management[edit | edit source]
- Pheochromocytoma is a surgical disease. Complete resection of the tumor is advised whenever possible
- There is no level 1 evidence exists regarding optimal preoperative or perioperative management
General principles (4):[edit | edit source]
- Pre-operative cardiology or anesthesia consultation because of risk for cardiomyopathy
- Preoperative cardiac workup, including electrocardiography and echocardiography, and assessment of hypertension-induced end-organ dysfunction are indicated.
- Restoration intravascular volume
- Pre-operative medications (α-Blockade followed by β-blockade)
- Monitored bed post-operatively
Restoration intravascular volume[edit | edit source]
- Most important component of preoperative management
- Most centers admit patients the day before surgery and initiate aggressive IV fluid resuscitation
Pre-operative medications[edit | edit source]
- Indications
- All patients with pheochromocytoma and an abnormal metabolic evaluation undergo preoperative catecholamine blockade, including patients who do not exhibit evidence of blood pressure elevation and lack classic symptomatology.
- Catecholamine release during intraoperative tumor manipulation can result in hazardous blood pressure elevation and cardiac arrhythmias.
- Recent data suggest that preoperative α-blockade may not be necessary in normotensive asymptomatic patients
- All patients with pheochromocytoma and an abnormal metabolic evaluation undergo preoperative catecholamine blockade, including patients who do not exhibit evidence of blood pressure elevation and lack classic symptomatology.
- α-Blockade
- Helps in both hemodynamic and glucose control
- Phenoxybenzamine
- Most common α- blocker used for preoperative catecholamine blockade of pheochromocytoma.
- MOA: irreversible, non-selective α receptor blocker
- Intraoperative catecholamine surges typically do not override its actions, because reversal of the blockade is possible only through synthesis of new receptor molecules.
- Non-selective nature may lead to tachycardia and β-adrenergic blockade may be necessary
- Prolonged hypotension in the immediate postoperative period and central nervous system effects such as somnolence may be expected
- Newer selective and competitive α1-adrenergic blockers such as doxazosin, prazosin, and terazosin obviate the drug-induced need for β-blockade.
- Started 7-14 days before surgery.
- Can be started at 10 mg twice daily with a stepwise increase of 10 to 20 mg every 2 to 3 days until a final dose of 1 mg/kg if tolerated.
- During this time blood pressure checks should be conducted at least 3 times a day.
- The last dose of phenoxybenzamine is usually given on the night before surgery, and the next morning’s dose is withheld to minimize potentially prolonged hypotension after tumor resection.
- Can be started at 10 mg twice daily with a stepwise increase of 10 to 20 mg every 2 to 3 days until a final dose of 1 mg/kg if tolerated.
- If phenoxybenzamine not effective for blockade, start metyrosine
- MOA of metyrosine: blocks the biosynthesis of catecholamines by inhibiting the conversion of tyrosine to L-dopa
- Generally added for extensive disease with large increases in catecholamines.
- Acute hypertensive attacks can also be treated with a short-acting alpha blocker such as phentolamine.
- β-blockade
- Must be given with caution in patients with myocardial depression
- Should never be started before appropriate α-blockade
- In the absence of α-blockade, β antagonists cause a potentiation of the action of epinephrine on the α1 receptors, resulting in hypertension, owing to blockade of the arteriolar dilation at the β2 receptor. For this reason, selective β1 adrenoreceptor blockers, such as atenolol and metoprolol, are usually preferred.
- May be added when (2)
- Systolic blood pressure is <100 mmHg
- Tachycardia or reflex tachycardia develops.
- Calcium channel blockers
- Some studies report that sole use of calcium channel blockers is sufficient for safe pheochromocytomas resection. This approach avoids the reflex tachycardia and postoperative hypotension that are seen with use of phenoxybenzamine. This strategy be reserved for patients who are normotensive with paroxysmal hypertension and a normal baseline blood pressure.
- Usually, preoperative calcium channel blockade for 2 weeks is sufficient.
Monitored bed post-operatively[edit | edit source]
- In the immediate postoperative period, consider overnight ICU admission for active monitoring
- If phenoxybenzamine was used for preoperative α-blockade, hypotension is common, given the lasting effects of the agent. Moreover, in a high catecholamine state, α2-adrenoreceptor stimulation inhibits insulin release. The withdrawal of this adrenergic stimulus after tumor resection may result in rebound hyperinsulinemia and subsequent hypoglycemia
Post-operative follow-up[edit | edit source]
- Repeat metabolic testing should be performed ≈2 weeks after adrenalectomy to document normalization of catecholamine levels
- Postoperative cross-sectional imaging is reasonable to document tumor resection and appropriate healing of the resection bed.
- Subsequent imaging should be guided by results of biochemical testing
- Annual biochemical follow-up is mandatory for all patients with resected pheochromocytoma.
- Lifelong screening for recurrence is recommended
- 10-year recurrence rates are as high as 16%.
- No consensus on follow-up protocols exists.
- In a patient with persistent hypertension 2-3 months after adrenalectomy, residual tumor somewhere else in the body must be considered. The patient should initially have plasma free metanephrine levels measured. If this is abnormal, MIBG scan may be helpful in identifying the location of this lesion.
Special Scenarios[edit | edit source]
Treatment of Hereditary Pheochromocytoma[edit | edit source]
- Given that for patients with MEN-2 and VHL, the risk of malignancy is low whereas the risk of bilateral disease is significant, partial cortical-sparing adrenalectomy has been advocated. This strategy is used to avoid lifelong hormonal replacement, with its associated morbidity
Treatment of Malignant Pheochromocytoma[edit | edit source]
- Currently, malignant pheochromocytoma can only be defined by the presence of clinical metastases.
- A number of pathologic criteria to differentiate benign from malignant disease have been proposed, but to date there is no criterion agreed on.
- Currently therapy for metastatic pheochromocytoma is largely palliative.
- Surgical metastasectomy of resectable disease is the standard of care
- Little evidence exists to demonstrate that it prolongs patient survival or is more effective for symptomatic relief than medical treatment with α/β-blockade and α-methyl-p-tyrosine
- Chemotherapy is primarily used in patients in whom MIBG therapy has failed or in those whose tumors do not demonstrate MIBG uptake on initial MIBG imaging studies.
Treatment of Pheochromocytoma in Pregnancy[edit | edit source]
- In a late term pregnancy, the patient should be treated with alpha-adrenergic blockade with phenoxybenzamine until the fetus has reached maturity to manage the hypertension. At this point, she should undergo caesarean section and tumor resection in one operation. The patient should not undergo the stress of vaginal delivery.
Questions[edit | edit source]
- Where can extra-adrenal pheochromocytomas originate from?
- List clinical manifestations of a pheochromocytoma
- What laboratory test do the CUA guidelines recommend to rule out primary pheochromocytoma?
- What is the gold standard imaging for pheochromocytoma?
- List the hereditary forms of pheochromocytoma
- Describe the key aspects of pre- and post-operative management of pheochromocytoma
Answers[edit | edit source]
- Where can extra-adrenal pheochromocytomas originate from?
- List clinical manifestations of a pheochromocytoma
- What laboratory test do the CUA guidelines recommend to rule out primary pheochromocytoma?
- What is the gold standard imaging for pheochromocytoma?
- List the hereditary forms of pheochromocytoma
- Describe the key aspects of pre- and post-operative management of pheochromocytoma
- Alpha blockade x7-14 days prior to surgery +/- deferred start of beta-blocker if patient develops tachycardia
- Restoration intravascular volume, consider admitting the day before surgery
- Post-op ICU admission to monitor for hypotension, hyperinsulinemia and resulting hypoglycemia
References[edit | edit source]
- Wein AJ, Kavoussi LR, Partin AW, Peters CA (eds): CAMPBELL-WALSH UROLOGY, ed 11. Philadelphia, Elsevier, 2015, chap 65
- Daneshvar M, Bratslavsky G. 2019 AUA Update on Pheochromocytoma.